A brain bleed (intracranial hemorrhage) is a type of stroke. It causes blood to pool between your brain and skull. It prevents oxygen from reaching your brain. It’s life-threatening and requires quick treatment for the best outcome. Contact 911 if you experience a sudden headache, confusion and numbness on one side of your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
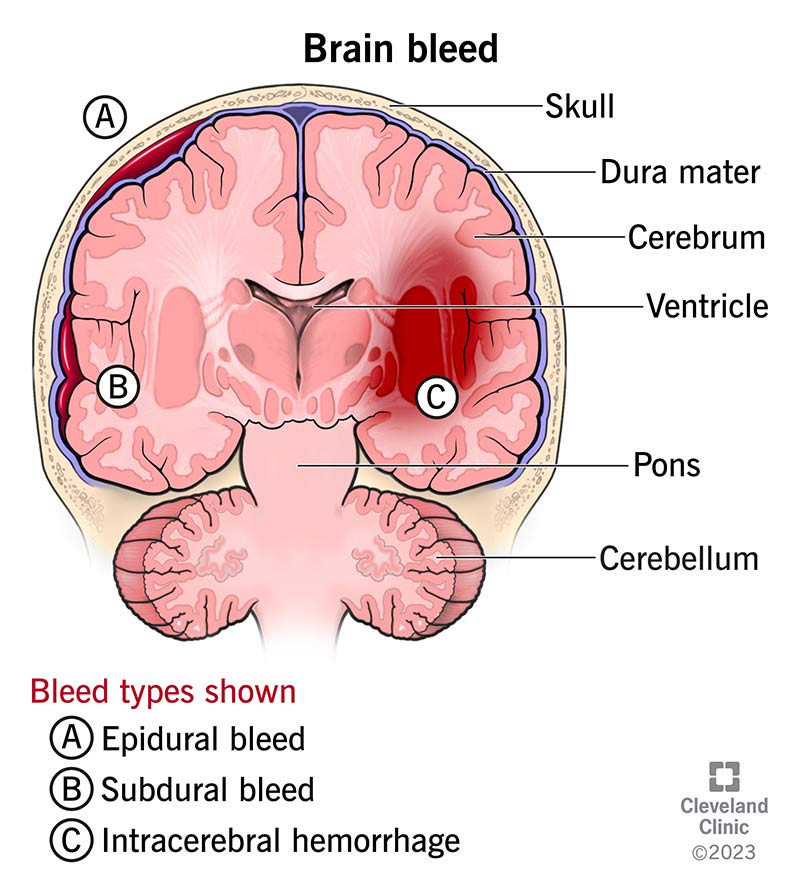
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/14480-brain-bleed-hemorrhage-intracranial-hemorrhage)
A brain bleed (intracranial hemorrhage) is a type of stroke that causes bleeding in your head.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As your brain can’t store oxygen, it relies on a series of blood vessels to supply its oxygen and nutrients. When a brain bleed occurs, a blood vessel leaks blood or bursts. Blood collects or pools within your skull and brain. This causes pressure against your brain, which prevents oxygen and nutrients from reaching your brain tissues and cells.
Brain bleeds are common after falls or traumatic injuries. They’re also common in people with unmanaged high blood pressure.
A brain bleed is a life-threatening medical emergency. It only takes three to four minutes for your brain cells to die if they don’t receive enough oxygen. Treating a brain bleed quickly leads to the best outcome.
There are many parts to your brain, so the term “brain bleed” (intracranial hemorrhage) is very broad to healthcare providers. Types of brain bleeds help your healthcare provider identify specifically where the bleeding occurs.
There are two main areas of bleeding:
To better understand where each type of brain bleed occurs, it helps to know the components within your skull. The brain has three membrane layers (meninges) between the bony skull and brain tissue. The three membranes are the dura mater, arachnoid and pia mater. The purpose of the meninges is to cover and protect your brain. Bleeding can occur anywhere between these three membranes.
Advertisement
Types of brain bleeds within your skull but outside of brain tissue include:
There are two types of brain bleeds that occur inside the brain tissue itself:
Brain bleeds can be life-threatening and cause permanent brain damage. The severity and outcome of a brain bleed depend on its cause, location inside of your skull, size of the bleed, the amount of time that passes between the bleed and treatment. Once brain cells die, they don’t come back. Damage can be severe and result in physical, mental and task-based disability.
Brain bleeds are a type of stroke. More than 795,000 people in the United States experience a stroke each year.
Symptoms of a brain bleed vary based on the type, but could include:
In addition, you may experience:
Most people who experience a brain bleed note that the first symptom is a sudden, painful headache.
A leaky, broken or burst blood vessel causes a brain bleed. As a result, excess blood pools in your brain. A brain bleed can happen after:
A brain bleed can affect anyone at any age, from newborns to adults. It’s more common among adults over age 65. You may be more at risk of a brain bleed if you experience the following:
Advertisement
If not treated quickly, a brain bleed can lead to permanent brain damage or death. A lack of oxygen to your brain can destroy your brain cells and prevent them from communicating with other parts of your body. This affects how your body functions overall, so you may experience:
A healthcare provider will diagnose a brain bleed after an immediate physical exam, neurological exam and testing. They’ll review your complete medical history and your symptoms first. Then, they’ll order an imaging test like:
Advertisement
These imaging tests determine the location, extent and, sometimes, the cause of the bleed.
Other tests can help detect a cause and may include:
Treatment for a brain bleed varies based on the severity and location of the bleed. Your healthcare provider will focus on stopping the bleeding and managing the cause. Treatment may include:
Prompt medical treatment can limit damage to your brain, which will improve your chance of recovery. In addition, you may receive:
Surgery can treat a brain bleed to stop bleeding and address the underlying cause. Surgery may include:
Advertisement
Some brain hemorrhages don’t require surgery. The decision depends on the bleed’s size, cause and location, along with other factors like your general health.
Based on your diagnostic test results, a healthcare provider may prescribe the following medications to treat the symptoms, the underlying cause or prevent complications of a brain bleed:
Each type of treatment comes with possible side effects. Due to the urgent nature of treatment for a brain bleed, you may need emergency treatment to prevent life-threatening complications.
Surgery comes at a higher risk due to the proximity of the procedure to your brain. Your highly trained surgical team will use caution to prevent possible complications.
You may need rehabilitation after a brain bleed. Depending on the severity of the bleed, brain damage is a possibility that can affect your ability to complete your daily routine. Rehabilitation can help you regain the functions needed for daily living and prevent future brain bleeds.
Long-term rehabilitation treatment may include:
Rehabilitation and recovery time vary according to each person’s situation.
Depending on the brain bleed’s location and the extent of damage, there can be lasting effects. Rehabilitation can help you manage these effects so you can complete your daily routine safely.
Unfortunately, a brain bleed can cause permanent damage, including paralysis, coma and death. Each situation is different, so a healthcare provider will be able to give you the most up-to-date information about your situation.
Remember, if you suspect a brain bleed, the sooner you get to the emergency room, the better your chance of survival. Don’t hesitate if you suspect something’s wrong. Let a healthcare professional determine if you have a brain emergency.
Your chance of survival after a brain bleed depends on the severity of the bleed, the amount of time between the start of the bleed and treatment, your overall health and other factors. If treated at the first sign of a brain bleed, your odds of survival are good.
Studies show that stroke is the third leading cause of death in the United States. While a stroke is a common cause of death, not everyone who experiences a stroke has life-threatening complications.
A healthcare provider can give you the most accurate information about your or your loved one’s chances of survival.
You can’t prevent all causes of brain bleeds, but you can take steps to reduce your risk by:
You can also protect yourself from injury by wearing protective equipment, like a helmet, during certain activities or wearing a seatbelt in vehicles.
Any type of bleeding inside of your skull or brain is a medical emergency. If you or a loved one experienced a head injury (blow to the head) or have symptoms that may indicate a brain bleed, like a sudden headache, confusion or numbness, call 911 or your local emergency services number. It’s important to get to a hospital emergency room immediately to determine the cause of your symptoms and to begin medical treatment.
A hemorrhage means bleeding caused by a damaged blood vessel. An intracranial hemorrhage is bleeding within your skull. An intracerebral hemorrhage is bleeding within brain tissue.
A brain bleed is a life-threatening medical emergency. It’s essential that you get help immediately to treat this condition before it causes permanent brain damage or death. It can be a scary situation for people who experience this type of stroke, as well as anyone caring for a person going through a stroke. Contact emergency services immediately after a fall or head injury. Look for signs of stroke, like a sudden and/or painful headache, numbness or weakness on one side of your body and confusion. Your outcome improves with a quick diagnosis and treatment, followed by rehabilitation if necessary.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
