Transverse myelitis (TM) is a rare neurological condition caused by inflammation of your spinal cord. It often results in sudden symptoms, such as muscle weakness, pain and bladder dysfunction. It has several possible causes. Some people recover from the symptoms and resulting complications of TM, while others don’t.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
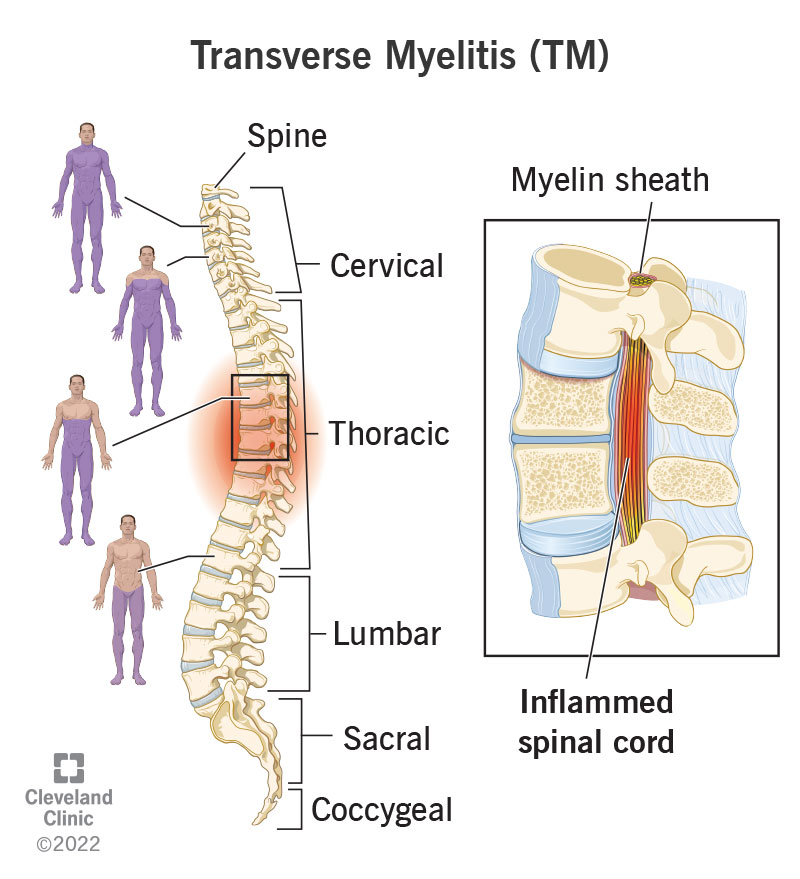
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/8980-transverse-myelitis)
Transverse myelitis (TM) is a rare neurological condition caused by inflammation of your spinal cord.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your spinal cord is a cylindrical structure that runs through the center of your spine, from your brainstem to your low back. It’s a delicate structure that contains nerve bundles and cells that carry messages from your brain to the rest of your body.
Due to inflammation, the covering (myelin sheath) around the nerve cells in your spinal cord is damaged. This interrupts the signals between spinal nerves and the rest of your body, causing issues such as loss of sensation, movement and bladder control.
TM can happen around your spinal cord in any region along your spine.
The term “myelitis” means inflammation of the spinal cord. “Transverse” refers to the pattern of changes in sensation and function — there’s often a band-like sensation across the trunk of your body in TM, with sensory changes below that band.
In most cases, TM is a one-time condition with a sudden onset followed by improvement or stabilization.
Transverse myelitis (TM) can occur in any person at any age. But it seems to affect people between the ages of 10 to 19 years, and 30 to 39 years more. Approximately 25% of cases affect children. TM doesn’t appear to be genetic or run in families.
Transverse myelitis is rare. There are approximately 1 to 8 new U.S. cases per 1 million people a year, or approximately 1,400 new cases each year.
Advertisement
Symptoms of transverse myelitis may develop within a few hours or days (have sudden onset), or they may develop over one to four weeks. Symptoms of TM can quickly become severe.
Symptoms of TM tend to happen at or below the damaged area of your spinal cord. For example, if the damaged area of your spinal cord is in your middle back below your arms, then your legs and bladder/bowel control will likely be affected, but your arms won’t.
TM often affects both sides of your body, but it sometimes only affects one side (this is more common in people with multiple sclerosis).
At its worst point, 50% of people with TM have lost all movements of their legs, 80% to 94% of people experience numbness or abnormal sensation (tingling or pricking), and almost all people have some degree of bladder dysfunction.
For some people, these symptoms improve or go away completely with treatment, whereas others experience permanent complications.
There are several different groups of symptoms for TM, including:
TM may cause the following abnormal sensations (paresthesia) in certain areas of your body, depending on where the damage is on your spine:
TM may cause pain in certain areas of your body. The pain may feel sharp or blunt. It may shoot (radiate) down your arms and/or legs or wrap around your chest and abdomen.
TM can cause the following bladder and bowel symptoms:
People with TM may have weakness in their legs that progresses rapidly. If the inflammation affects your upper spinal cord, it affects your arms as well.
Signs of muscle and movement issues include:
People with TM may experience difficulty having an orgasm, and people with a penis may experience erectile dysfunction.
TM can also have the following symptoms:
In general, transverse myelitis (TM) is caused by inflammation of your spinal cord.
When your body encounters an offending agent (like viruses, bacteria or toxic chemicals) or suffers an injury, it activates your immune system.
Advertisement
Your immune system sends out its first responders: inflammatory cells and cytokines (substances that stimulate more inflammatory cells).
These cells begin an inflammatory response to trap bacteria and other offending agents or start healing injured tissue. While this inflammatory response is necessary in a lot of cases, sometimes, your immune system can send out its first responders for no known reason and attack healthy tissue. Or the inflammatory response to an offending agent can be excessive and damage tissues in your body in the process.
In the case of TM, the covering around the nerve cells in your spinal cord is damaged due to inflammation.
There are several possible causes of inflammation that lead to transverse myelitis (TM). The causes can be grouped into the following categories:
Idiopathic TM means there’s no known cause of the condition. This represents the majority of TM cases.
Scientists think idiopathic TM results from an abnormal and excessive immune response against your spinal cord that results in inflammation and tissue damage. But they can’t figure out the exact cause or trigger.
Advertisement
Bacterial, viral, parasitic and fungal infections that can cause TM include, but aren’t limited to:
It’s often difficult for healthcare providers to determine whether direct viral infection or a post-infectious response from your immune system causes TM.
Systemic inflammatory autoimmune conditions that have an association with TM include:
Central nervous system autoimmune conditions that can cause TM include:
Advertisement
In some people, transverse myelitis represents the first symptom of a central nervous system autoimmune or immune-mediated condition, such as multiple sclerosis (MS) or neuromyelitis optica spectrum disorder (NMOSD).
“Partial” myelitis, which means only one side of your body is affected, is more common in MS.
NMSOD is much more likely as an underlying condition when the myelitis is “complete,” meaning it causes severe paralysis and numbness on both sides of your body. Myelitis attacks that happen to people with NMOSD tend to be more severe and are associated with less recovery than attacks in people with MS.
Rarely, people have reported receiving a vaccine two days to three months before developing transverse myelitis. Although scientists haven’t found the exact reason for the possible link between vaccines and transverse myelitis, one theory suggests that the vaccination may jumpstart an autoimmune process in certain people. It’s very important to know that extensive research has proven vaccinations are safe, and the potential link to TM may only be coincidental or, at worst, a rare complication.
If you’re experiencing symptoms of transverse myelitis (TM), your healthcare provider will review your medical history and perform a physical examination.
If this review suggests a problem with your spinal cord, they’ll order further tests to:
Healthcare providers diagnose TM if you develop spinal cord symptoms over a few days and magnetic resonance imaging (MRI) or other imaging doesn’t show another cause for the spinal cord issues.
Your healthcare provider may order the following tests to diagnose transverse myelitis and its cause:
You may need additional tests depending on the possible cause of TM. If none of these tests suggests a specific cause, you’re presumed to have idiopathic transverse myelitis.
The goals of treatment for transverse myelitis (TM) include:
Treatment for TM involves acute (short-term) treatment of the inflammation and its cause and long-term management of the complications TM may have caused.
The first-line treatment for transverse myelitis is IV (intravenous) glucocorticoids. If your healthcare provider suspects TM, they’ll start high-dose IV glucocorticoids as soon as possible.
Glucocorticoids are a class of corticosteroids, which are a class of steroid hormones. Glucocorticoids are powerful medicines that fight inflammation and work with your immune system. In the case of transverse myelitis, glucocorticoids help reduce the inflammation of your spinal cord.
You’ll likely be on these medications for at least three to five days, but you may need the medication for longer.
Additional treatments for TM may include:
After you’ve received treatment for the acute phase of transverse myelitis (TM), you’ll likely need rehabilitative care to improve functional skills and prevent secondary complications of TM.
Although rehabilitation can’t reverse the physical damage resulting from TM, it can help people, even those with severe paralysis, become as functionally independent as possible and have the best possible quality of life.
Long-term management of transverse myelitis may include:
Yes, you can recover from transverse myelitis (TM), but recovery looks different for different people.
Recovery from TM may be absent, partial or complete and generally begins within one to three months after initial treatment. Most people recover from transverse myelitis (TM) within three months after the condition happens. For some, healing may take months to years.
While some people recover from the inflammation with little or no lasting complications, others recover with moderate or severe disabilities.
Those who may have a poor chance of recovery include:
The outlook (prognosis) for people with transverse myelitis varies:
Transverse myelitis usually only happens once in most people. It may recur (happen again) in some people with an underlying cause, such as multiple sclerosis (MS). If only one side of your body was affected by TM, you may be more likely to develop MS in the future.
If you have transverse myelitis, it’s essential to ensure you’re getting quality medical care to prevent or treat complications of TM, such as bowel and bladder dysfunction and muscle tightness. You may also want to consider joining a support group to meet others who can relate to your experiences. It’s also important to seek help from a therapist or psychologist if you’re experiencing depression or anxiety related to TM.
If you’re taking care of someone with TM, it’s important to advocate for them to ensure they get the best medical care and access to mobility devices and therapy that can help them be more independent.
It can be difficult for you and your family to cope with the psychological and physical effects of TM. During the early recovery period, family education is essential to develop a plan for dealing with the challenges to independence.
If you’re experiencing symptoms of transverse myelitis, such as sudden and worsening muscle weakness and pain, get to the nearest hospital as soon as possible.
If you’ve been diagnosed with TM, you’ll need to see your team of healthcare providers regularly to receive therapy and monitor possible complications.
Understanding your or your loved one’s transverse myelitis (TM) diagnosis can be overwhelming. But your healthcare team will offer a robust treatment and rehab plan that’s unique to you or your loved one’s symptoms. It’s important to make sure you’re getting the love and support you need throughout your recovery and stay attentive to your health to address any new symptoms that arise.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
