Dilated cardiomyopathy causes tissue in your heart’s main pumping chamber to expand (dilate) and thin out. This makes it unable to pump as strongly as it should. Genetics or heart attack damage can cause this, but often, the cause is unknown. This condition can affect several chambers of your heart and lead to complications like heart failure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
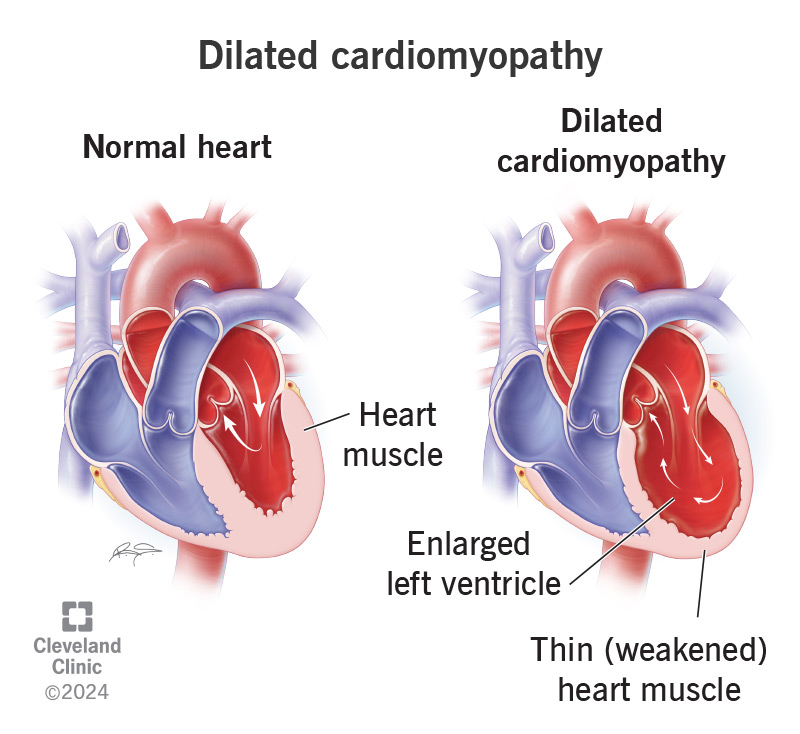
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16932-dilated-cardiomyopathy)
Dilated cardiomyopathy is an issue with your heart muscle stretching out and becoming larger than usual. It starts in your heart’s main pumping chamber (left ventricle). In severe cases, it affects more areas of your heart.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With increased wall stress, the tissue in your left ventricle becomes enlarged and then thins. This causes it to pump with less force than it should. After each beat, more blood remains in your heart. This makes it increasingly difficult to keep up with your body’s needs.
Researchers estimate that 36 people per 100,000 in the general population have dilated cardiomyopathy.
Fortunately, treatments are available for this heart condition. And there are things you can do to help manage this condition.
Many people with dilated cardiomyopathy don’t have any symptoms, especially in the early stages. But as heart function worsens, you may notice symptoms more and more.
Dilated cardiomyopathy symptoms may include:
In many cases, experts don’t know the cause. In others, dilated cardiomyopathy causes may include:
Advertisement
Some people have more than one cause. For example, you can be at risk because of genetics and then get a medical condition that leads to dilated cardiomyopathy.
You may be more at risk for dilated cardiomyopathy if you:
In advanced stages, dilated cardiomyopathy can lead to complications.
These complications may include:
A healthcare provider will start by taking your medical history and family history. They’ll perform a physical exam that may include listening to your lungs to check for fluid build-up. Your provider may hear a heart murmur before you even have symptoms.
Testing will determine the severity and help healthcare providers plan your dilated cardiomyopathy treatment.
Tests you may need include:
You may need a variety of dilated cardiomyopathy treatments. In most cases, they won’t cure the disease, but they can help you manage the symptoms and live longer. Treating dilated cardiomyopathy may involve medicines, changes to your lifestyle or surgeries. The earlier you start treatment, the better your prognosis (outcome). Your cardiologist or heart failure specialist will work with you to find the right combination of these medicines.
Medications that improve your heart function with dilated cardiomyopathy include:
Changes to your daily routine can improve how well medications work and possibly help you delay or avoid the need for a procedure.
These changes include:
Advertisement
You may need a procedure or surgery if you have advanced dilated cardiomyopathy and limited heart function. Procedures for dilated cardiomyopathy treatment include:
Your prognosis depends on the cause and severity of the disease. With ongoing care, you may return to work and your usual daily activities. But you may have symptoms that get worse with time. Advanced dilated cardiomyopathy or complications can make you severely ill. You may need to stay in the hospital until symptoms improve.
Dilated cardiomyopathy can get worse for many people and lead to long-term heart failure. This means your heart can’t keep up with the demands on it. Kidney failure and severe heart failure are signs of a poor prognosis (outcome). People who have symptoms at rest or can’t do physical activity tend to have the worst prognosis.
Advertisement
Still, the prognosis for people with dilated cardiomyopathy has improved in recent years. This is due to the treatments available and early diagnosis and treatment. Today, more than 80% of people with this condition are alive at their eight-year follow-up visit and don’t need a heart transplant.
It’s not always possible to prevent this condition. It may run in your biological family or be a side effect of a treatment like chemotherapy.
But you may be able to prevent dilated cardiomyopathy by:
You can care for yourself by following your provider’s instructions. These include:
Because your condition can change over time, your best game plan is to have regular visits with your provider. These visits should continue for the rest of your life. Contact your provider if the symptoms get worse. They can offer treatments that help you manage symptoms.
Advertisement
You may have lots of questions about a condition that’s new to you, like:
No one wants to learn that their heart isn’t working as well as it should. But today, healthcare providers can offer various treatments to help your heart work better if you have dilated cardiomyopathy. And there are simple changes you can make to improve your situation, too. Don’t be afraid to ask questions so you can understand your options. You can work with your provider to find a way forward.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic offers personalized diagnosis and the latest treatments for hypertrophic cardiomyopathy.
