Myocarditis is inflammation of the heart muscle, or myocardium. This inflammation weakens your heart muscle, making it harder for your heart to pump. This can be caused by viral infections or inflammatory conditions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
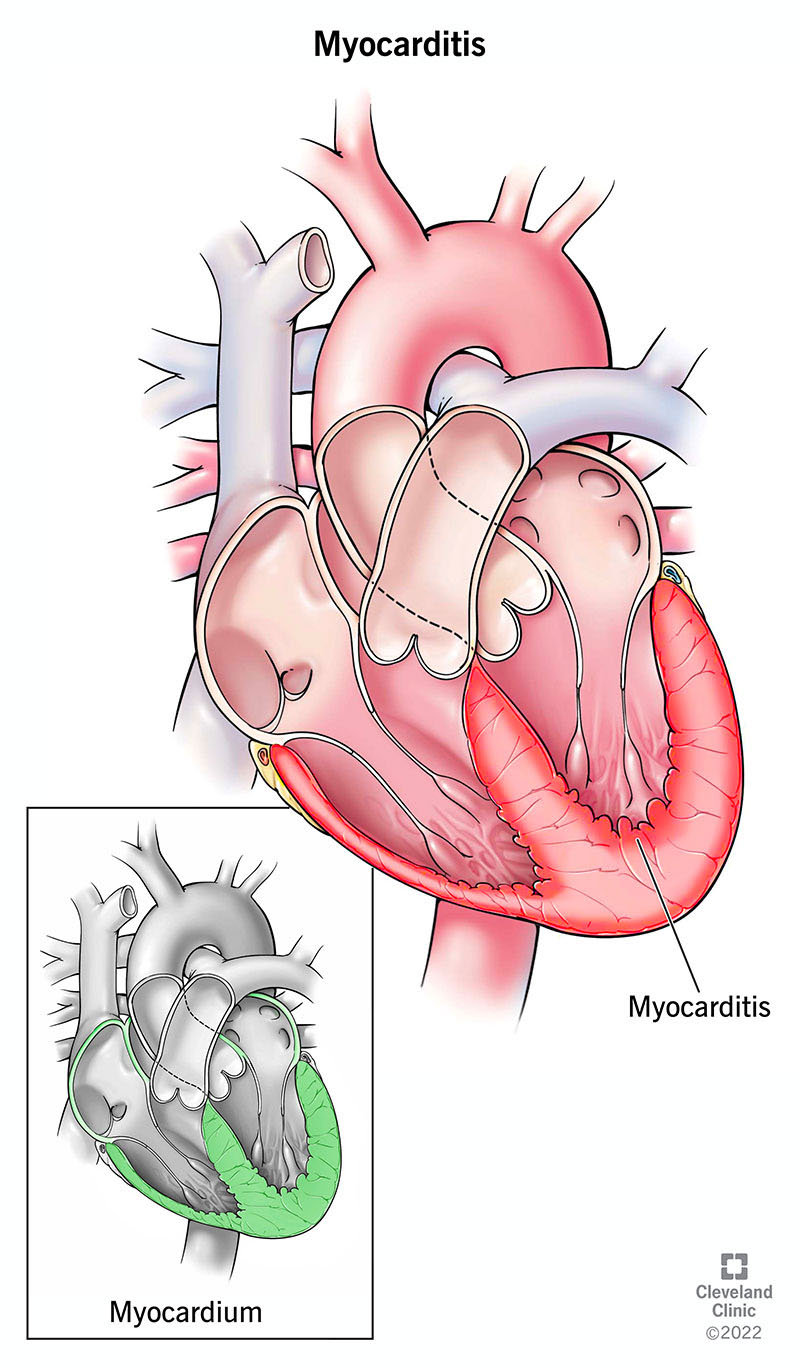
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22129-myocarditis)
Myocarditis is inflammation of your heart muscle (myocardium). This can weaken your heart muscle, making it more difficult for your heart to pump. This rare condition can affect people quickly or slowly over time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Myocarditis is different from other types of inflammation because each kind happens in a different part of your heart. Pericarditis affects the sac around your heart. Endocarditis is an infection or inflammation of your heart valves.
Rare types of myocarditis include:
People with myocarditis often feel fatigued, short of breath, chest pain or the sensation of their heart racing (palpitations). They may feel these symptoms gradually over time, or their symptoms may happen very quickly. People with myocarditis in more advanced stages may show symptoms of heart failure.
Researchers estimate there are about 1.5 million cases of myocarditis in the world each year. This works out to 10 to 20 people affected out of every 100,000 people.
You may have no symptoms, few symptoms or many symptoms, and they may be more severe in some people than in others. Myocarditis symptoms include:
Many times, the cause of myocarditis is unknown. Most often, the cause is a viral infection. These include:
Advertisement
Other causes of myocarditis include:
Side effects from some medicines can bring about myocarditis. These medicines include:
In rare cases, myocarditis has happened in young people who received the Pfizer-BioNTech® or Moderna® vaccines for COVID-19. Symptoms can start during the first week after receiving the vaccine. Most people who have this reaction to the COVID-19 vaccine recover quickly after treatment and can get back to their regular activities when they feel better. But if you’ve had myocarditis, check with a cardiologist before starting to exercise again.
The CDC says the risk from COVID-19 is higher than the small risk of rare side effects like this, and continues to recommend the vaccine.
Some of the things that put you at risk for myocarditis can’t be changed. You’re more likely to get myocarditis if:
Some medical treatments increase your risk of myocarditis. These include:
Having one of these medical problems can put you at a higher risk of getting myocarditis:
In some people, myocarditis can bring on other issues, such as:
Your healthcare provider will use the following to diagnose myocarditis:
Your healthcare provider may order tests to help them decide if you have myocarditis or something else.
These tests include:
Advertisement
If you have a mild case, it may go away on its own. If not, your provider can order medicines for you.
To treat myocarditis, your healthcare provider may want you to take medication. These include:
If your myocarditis led to heart failure or an abnormal heart rhythm and your case is serious, you may need surgery to implant a:
Your prognosis with myocarditis depends on how severe your symptoms are and how inflamed your heart is. Many people can live for years without problems after treatment for myocarditis. Others may need to keep taking medications. There’s also a small risk that you’ll develop myocarditis again.
For some people, myocarditis can lead to serious complications like dilated cardiomyopathy, a condition where the heart becomes enlarged and weak. This can eventually lead to heart failure, and they may need a heart transplant. Myocarditis is also linked to nearly 20% of sudden deaths in young people. While many people recover, it can still be life-threatening.
About 50% to 80% of those with viral myocarditis survive five years or more after diagnosis. Many people, especially younger people, recover fully and go on to live healthy, active lives.
Advertisement
Unfortunately, it’s very hard to avoid many of the things that cause myocarditis. Your best bet is to wash your hands often and stay healthy to keep from getting infections that can bring about myocarditis. It’s also important to stay up to date on the flu vaccine. Limiting your alcohol intake and not taking prohibited drugs are other risk factors you can manage.
Once you’ve had myocarditis, you can get it again years later. Tell your provider if you get symptoms again. For your best chance of staying healthy:
Also, they may want to repeat some tests used for diagnosis. These include:
Myocarditis is a rare condition that can weaken your heart muscle. Unfortunately, there are many causes of myocarditis that are hard to avoid. While symptoms can be severe in some people, many people can live for years without myocarditis becoming a problem again after treatment. The best thing you can do is keep your follow-up appointments with your provider, keep taking the medicines they prescribed for you and let them know if you get symptoms again.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
