Rheumatic heart disease is a condition with heart valve damage from rheumatic fever. This can happen after an untreated strep infection. People in countries without access to antibiotics are at the highest risk. The condition can lead to serious health problems like heart failure. Medication and surgery are the main treatments, but not a cure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
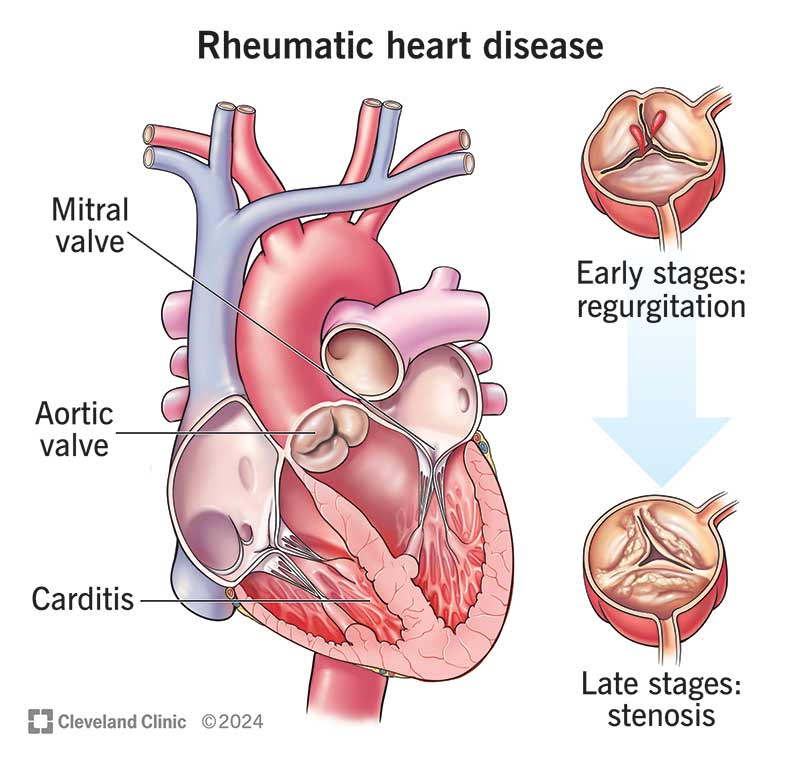
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/rheumatic-heart-disease.jpg)
Rheumatic heart disease is heart valve damage from rheumatic fever. Bacterial infections called group A streptococcal (GAS) infections can cause rheumatic fever. An infection like strep throat or scarlet fever triggers your body’s immune response, causing inflammation throughout your body, including in your heart.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Inflammation from rheumatic fever can lead to permanent damage to your heart valves. Your valves keep your blood flowing in the right direction through your heart. Damaged valves reduce the amount of blood that can move through your heart. They also may allow some blood to go in the wrong direction.
Rheumatic heart disease is rare in the U.S. It’s more common in low-income or developing parts of the world where people can’t get antibiotics for bacterial infections. About 300,000 people worldwide die of rheumatic heart disease each year. More than 40 million people in the world have the disease.
Children and teenagers with untreated strep infections are the most likely to get rheumatic fever, often between ages 5 and 15. Signs of heart damage can develop years after the infection and fever are gone. People often show signs of rheumatic heart disease as young adults.
Some people may have symptoms of heart involvement during an acute episode of rheumatic fever. But in most cases, rheumatic heart disease symptoms may not appear until years after a strep infection or rheumatic fever. People with heart damage may experience:
Advertisement
Heart valve inflammation from rheumatic fever causes rheumatic heart disease. The damage may happen right away. Or it can develop over time from repeated strep infections. Continuing inflammation leads to heart valve scarring and narrowing.
Rheumatic heart disease isn’t contagious. But strep throat is. This infection can lead to rheumatic fever, the cause of rheumatic heart disease.
People are at a higher risk for this disease if they:
Rheumatic fever can affect your heart about 20 or 30 years after an episode of rheumatic fever. If you had repeated episodes or were younger when you had rheumatic fever, you may see the consequences of rheumatic heart disease at a younger age.
One or more of your heart valves can grow narrow (referred to as stenosis of the valve) or allow blood to flow backward in the wrong direction. Providers call this regurgitation. Rheumatic heart disease tends to affect the mitral and aortic heart valves.
Rheumatic heart disease can lead to:
Some of these conditions can increase your risk of stroke or blood clots.
Rheumatic heart disease is especially dangerous if you're pregnant. Pregnancy increases the amount of blood in your body. Your heart has to work harder to pump the extra blood. As a result, a woman with damaged heart valves can have serious health issues during pregnancy. The fetus’s health is also at risk.
To diagnose rheumatic heart disease, a healthcare provider will evaluate your symptoms and perform a physical exam. They’ll also review your health history, especially any history of fevers or bacterial infections.
Your provider may use the following tests to diagnose rheumatic heart disease:
Rheumatic heart disease treatments can help you manage symptoms and may delay disease progress. But they can’t cure the condition. Treatments include:
Advertisement
The right treatments may delay or prevent heart failure in people with rheumatic heart disease. But the disease is permanent and requires long-term care. Without regular checkups, rheumatic heart disease can lead to severe heart failure.
The length of time that you can live with rheumatic heart disease depends on how severe it is at diagnosis. In a study of indigenous people in Australia under 25, those who had severe rheumatic heart disease at diagnosis got worse fairly quickly. Of this group, 50% had surgery within two years and 10% of them died within six years after their diagnosis.
Some people with moderate disease improved, while others stayed the same or got worse. Ten years after diagnosis, 60% of people with mild rheumatic heart disease didn’t get worse.
Yes. You can prevent rheumatic heart disease by taking antibiotics at the first signs of a streptococcal infection. See your healthcare provider if you or your child has:
People at risk of rheumatic heart disease may need penicillin injections every three to four weeks for five or more years or lifelong, depending on the degree of heart involvement. This can also keep rheumatic heart disease from getting worse by preventing the infection that causes rheumatic fever.
Advertisement
If you have rheumatic heart disease, you should avoid getting rheumatic fever again. It can make your heart disease worse. Your provider can monitor your health to make sure you get antibiotics if you get strep throat again. You may also be able to receive antibiotics to prevent the strep infection that causes rheumatic fever.
Follow your provider’s instructions for treating rheumatic heart disease. That may include taking medicines, going to follow-up appointments or having surgery.
Contact your provider if you experience new or worsened symptoms, including:
Questions to ask your healthcare provider may include:
Maybe you couldn’t do anything about the strep infections you had as a child. But you can do something now about rheumatic heart disease. Take charge of your health by talking with a healthcare provider about the best ways to treat your heart issue and stay safe from another infection. The best thing you can do for your health is to follow a provider’s advice for staying healthy.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
