Pulmonary artery stenosis (narrowing) affects the artery that carries blood to your child’s lungs to pick up oxygen. To make up for this limited blood flow, right ventricle pressure can go high enough to injure heart muscle. Several different treatments can work, but your child may need another procedure later.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
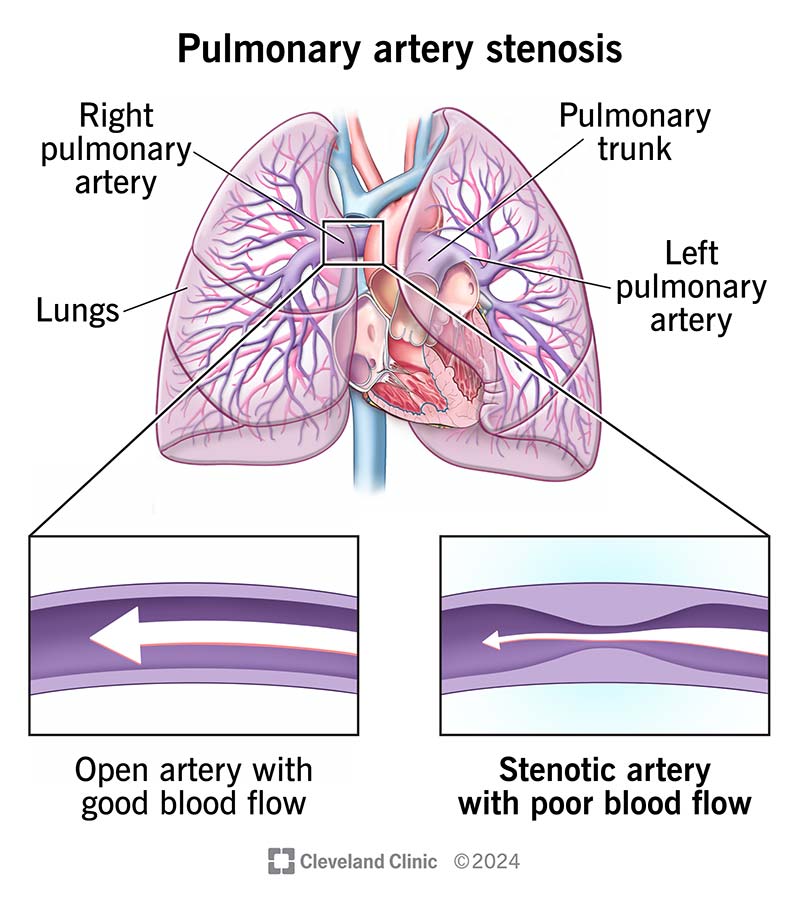
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17399-pulmonary-artery-stenosis-illustration)
Pulmonary artery stenosis is narrowing in the pulmonary artery, a large blood vessel that connects the right ventricle to the lungs. In the lungs, blood picks up oxygen to carry to the body. Narrowing in the pulmonary artery makes it hard for blood to reach your child’s lungs. Without enough oxygen, your child’s heart and body can’t function as they should.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Narrowing may occur in the main pulmonary artery and/or in its left or right branches. When this occurs, the right ventricle must work harder to pump blood across the narrowing. Over time, this can cause damage to the heart muscle.
Without treatment, this condition can lead to right-sided heart failure.
Pulmonary artery stenosis is relatively rare. It may affect children who were born with other heart issues (congenital heart disease), or it can occur in isolation (without other heart defects). It also may develop after certain heart surgeries.
Symptoms depend on the severity of the stenosis (narrowing). If the narrowing is mild, your child may not have symptoms. As the narrowing becomes severe, your child may experience the following:
Some people are born with pulmonary artery stenosis and have problems with their heart valves, walls or other parts of their heart as well. Others who have pulmonary artery stenosis at birth have no other heart issues. You can also develop the condition after heart surgery or from diseases that aren’t very common.
Advertisement
In 40% of cases, people are born with pulmonary artery stenosis but don’t have other heart problems.
Pulmonary artery stenosis happens in 2% to 3% of people who have other congenital (since birth) heart defects, such as:
Other causes of pulmonary artery stenosis can include issues such as:
Some people get pulmonary artery stenosis after having a surgical procedure. These include:
Your child’s healthcare provider may hear abnormal heart sounds (a murmur) during an exam. If this happens, they’ll order other tests that can include:
Advertisement
If your child’s healthcare provider diagnoses them with pulmonary artery stenosis, they’ll recommend that you meet with a congenital heart specialist. This type of provider has the training and equipment to determine your child’s heart problem and order the necessary special tests, medical care, heart surgery and follow-up checkups. They may order additional tests as necessary.
Your child’s provider may talk about their condition in terms of a Type I, II, III or IV. These are categories based on how many parts of the artery are narrow and where these spots are located.
The best treatment approach will depend on your child’s symptoms and other factors. Mild to moderate narrowing in one or more pulmonary artery branches usually doesn’t require treatment. However, severe cases need treatment.
Pulmonary artery stenosis treatments include:
Your child’s provider will:
Your child’s provider will:
Advertisement
This balloon is similar to a standard one. However, the balloon has small blades running up and down its length. When your child’s surgeon inflates the balloon, they activate the blades, which cut through the narrowed area. This makes the vessel easier to dilate and results in a larger opening.
This option gives good results for many people who don’t have an associated congenital heart problem. However, the artery can become narrow again in as many as 21% of people over several months.
Surgeons use various methods to repair pulmonary artery stenosis. The choice depends on what the stenosis is like. They also look at the surrounding vessels and other structures.
Balloon dilation improves narrowing in a majority of people. However, over time, the artery can become narrow again in as many as 15% to 20% of cases. This means your child’s provider will need to do the procedure again. Researchers are working on different types of balloons that will likely lead to better and longer-lasting results.
Balloon dilation complications include:
It can also be fatal.
Complications of stent use include:
Advertisement
Healthcare providers prefer stents for pulmonary artery stenosis because they:
Providers may choose balloon angioplasty instead of a stent when:
If your child receives a stent, they’ll take antibiotics and possibly blood thinners for a while. These medicines prevent infections and blood clots.
Procedures to expand your child’s pulmonary artery work right away. This means your child will have an easier time getting blood to their lungs to get oxygen.
With today’s advances in medical treatment, many people with this condition live to be adults. However, people with conditions like Williams syndrome and Alagille syndrome don’t respond as well to treatments.
Your child will need regular checkups with their provider to see how they’re doing. Also, they’ll need regular echocardiograms to see if their artery needs to be expanded again in the future.
If your child needs treatment for pulmonary artery stenosis, their healthcare provider will consider the best treatment for your child’s situation. You should feel comfortable asking questions about anything you don’t understand about your child’s procedure.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Congenital heart disease in children comes with a lot of questions and concerns. Cleveland Clinic Children’s has the answers and support you need.
