Alagille syndrome is a condition you’re born with that causes malformed, narrowed or missing bile ducts. This can make bile back up and collect in your liver. It can lead to liver damage and vitamin deficiencies. It can also affect your heart and other organs. Some symptoms include dark pee, pale poop, itching and yellowish skin or eyes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Alagille syndrome is a genetic condition that causes narrowed, malformed or missing bile ducts. Bile ducts are the tubes that carry bile (fluid that helps break down fats) from your liver to your gallbladder and intestines. Malformed, narrowed or missing bile ducts can make bile to back up into your liver, damaging it. It can also lead to low levels of vitamin A, vitamin D, vitamin E and vitamin K in your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Alagille syndrome can affect other parts of your body, too. It can cause:
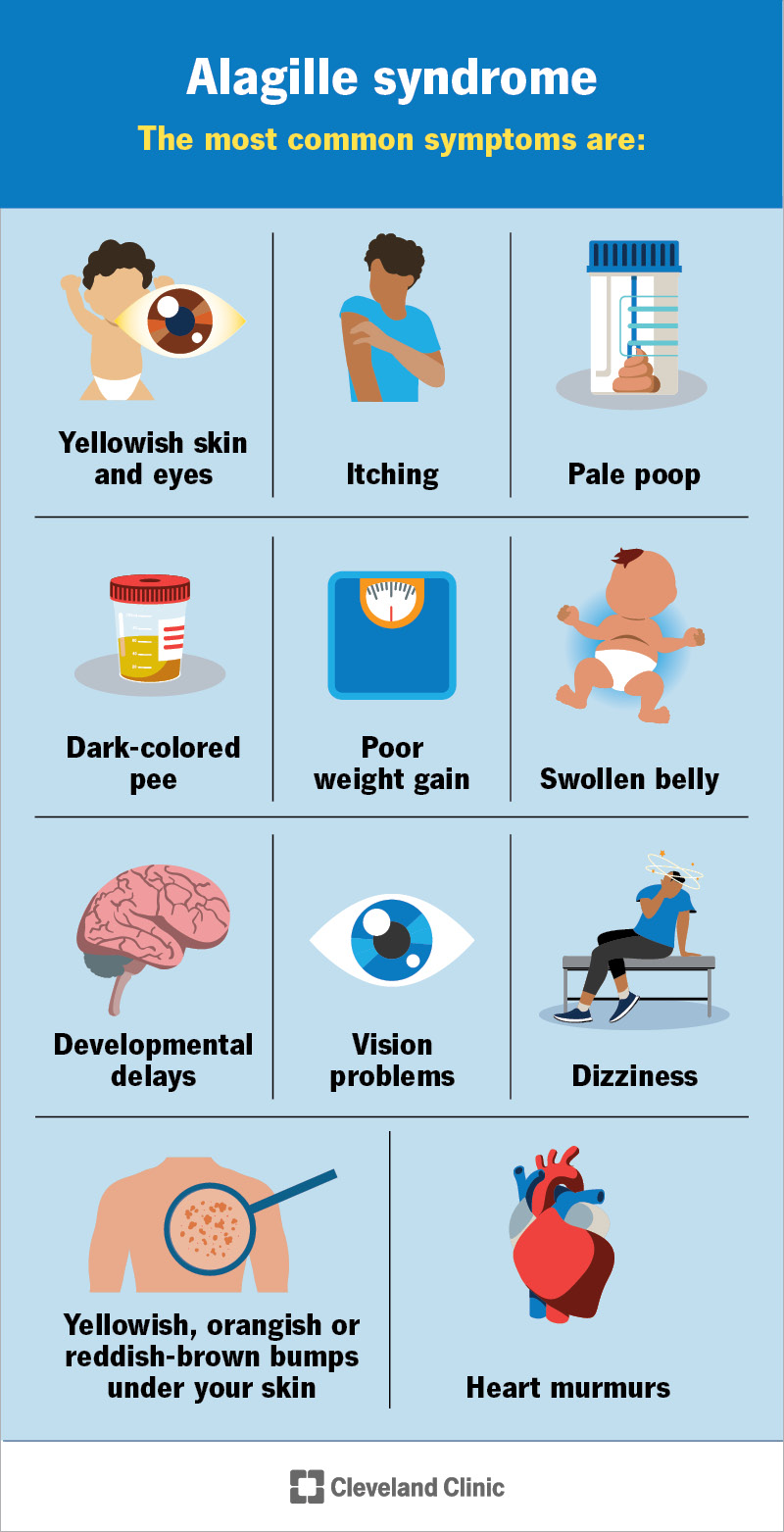
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23540-alagille-syndrome)
Symptoms could include:
Some kids may also have symptoms of heart conditions, like heart murmur, dizziness, shortness of breath, chest pains and bluish or grayish skin, lips or nails.
Symptoms of Alagille syndrome can be different for each person. They might be mild or severe, and some people might just have one or two of the features. It even affects members of the same family differently. The first symptoms you might notice of Alagille syndrome in infants are dark pee, light poop, a swollen belly and jaundice (that lasts several weeks after birth).
Advertisement
A harmful change in the DNA that makes up one of two genes causes Alagille syndrome. You or your child might have inherited this change from a biological parent. Or it might happen without any family history due to a new change in the person with Alagille (60% of the time). Most people (97%) with Alagille syndrome have a change in either the JAG1 or NOTCH2 gene.
These gene changes affect how organs and bones form. It can cause bile ducts that are too narrow or don’t form like they should. Or one or more bile ducts could be missing. This means that bile can back up and collect in your liver, damaging it. The lack of bile in your digestive tract means you aren’t able to absorb fats and certain vitamins.
Your heart valves and blood vessels can also narrow. This can keep blood and oxygen from getting to your tissues and organs.
Complications of Alagille syndrome include:
Alagille syndrome can be difficult to diagnose because the symptoms vary from person to person. Sometimes, people are diagnosed as adults, but this usually happens in childhood.
A healthcare provider will start by asking about your child’s symptoms. They might suspect your child has Alagille syndrome if they have bile duct differences and at least three other signs of the condition (like bone, blood vessel or eye differences).
Your child’s provider will need to do some procedures and tests to confirm the diagnosis. These could include:
There’s no cure for Alagille syndrome. But you can treat the symptoms and reduce your risk or your child’s risk of complications. Treatment could include:
Talk to a healthcare provider if you or your child has Alagille syndrome and:
Advertisement
Some complications of Alagille syndrome can be life-threatening. Call 911 (or your local emergency number) or go to an emergency room right away if you or your child has:
Everyone’s a little bit different. Some people with Alagille will have mild symptoms, and some are at high risk for serious complications. Some children might take longer to crawl or walk. A small percentage will have intellectual delays or disabilities.
People with mild symptoms have a life expectancy similar to people without Alagille syndrome. People with more severe symptoms are at a higher risk for complications and might have a shorter life expectancy. Your healthcare provider can let you know what to expect for yourself or your child.
Since you’re born with Alagille syndrome, there’s no way to prevent it. If you or someone in your family has Alagille syndrome, you can talk to a genetic counselor before getting pregnant about the chances of your child inheriting it.
If your child is diagnosed with a lifelong condition, the future may feel uncertain. While there’s no cure for Alagille syndrome, you and your child’s provider can work together to manage symptoms. With these adjustments, many people with Alagille syndrome can lead active lives for as long as those without the condition.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Do certain health conditions seem to run in your family? Are you ready to find out if you’re at risk? Cleveland Clinic’s genetics team can help.
