Rubella is an illness caused by the virus RuV. It causes a rash, low fever and other symptoms. It’s highly contagious person-to-person. Pregnant women with rubella can pass it to the fetus, causing hearing and vision loss, heart defects and other serious conditions. Rubella is preventable by getting vaccinated.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
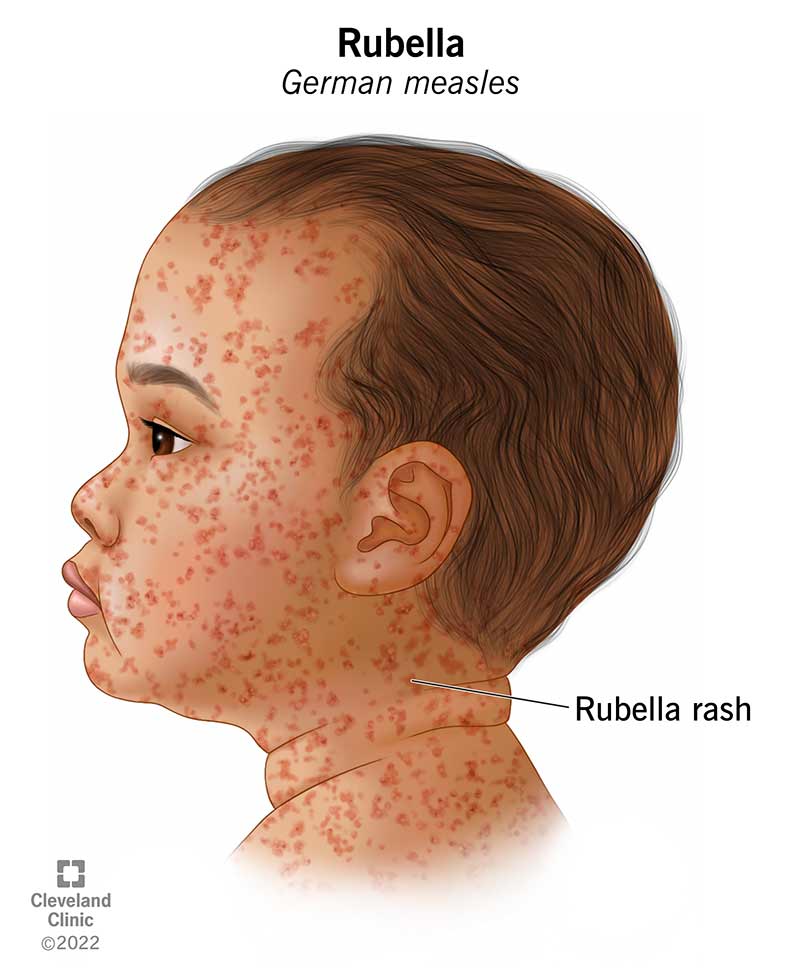
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/17798-rubella)
Rubella is a contagious illness you get from the RuV virus. It causes a rash that usually starts on your face and moves down your body. It can cause serious illness in newborns of women who had rubella while pregnant.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Rubella is also called German measles or three-day measles. Even though it causes a rash like measles, rubella happens because of a different virus than measles.
Congenital rubella syndrome (CRS) is the most serious form of rubella. It happens when a pregnant woman passes rubella to the fetus. This can cause skin, hearing, vision, heart and brain problems in newborns.
No, rubella and measles are different illnesses. They both give you a rash, but different viruses cause them.
Anyone can get rubella, but the most serious form of rubella, congenital rubella syndrome, affects newborns born to a woman who had rubella during pregnancy.
The U.S. eliminated rubella (meaning it’s no longer continuously spread) in 2004, but you can still get rubella in other parts of the world.
There are about 26,000 cases of rubella worldwide each year. It’s most common in Asia, Africa and the Middle East. There are only a few cases diagnosed each year in the U.S. since the disease’s elimination.
Rubella’s prominent symptom is a rash that usually starts on your face and moves down the rest of your body. In young children, a rash is often their first symptom. In older children and adults, the rash can appear a few days after other symptoms start.
Advertisement
Up to 50% of people have no symptoms at all but can still spread rubella to other people.
Symptoms of rubella include:
The cause of rubella is the RuV virus. Viruses are small shells with a genetic code inside (RNA or DNA). They use cell “machinery” from humans, animals or plants to make more copies of themselves.
Yes, rubella is contagious — it spreads from person to person when you cough, sneeze or touch surfaces with the virus on them. It can also spread from a pregnant woman to the fetus. You can be contagious with rubella without symptoms.
You’re contagious with rubella for about a week before and a week after the rash appears.
Yes, rubella is contagious and adults can get it from kids or other adults.
Rubella is most serious in pregnancy. If you’re pregnant and get rubella, especially in the first trimester, your child is at high risk for congenital rubella syndrome (CRS). CRS is preventable if you get vaccinated before getting pregnant.
If you’re not sick and your healthcare provider does a blood test for rubella before you get pregnant or while you’re pregnant, they’re looking for antibodies to rubella. Your body makes antibodies when it finds a harmful invader in your body.
If you test positive to a rubella antibody test, it means you either had rubella before or received a vaccination for it. Either way, you’re immune to rubella and are unlikely to get it while you’re pregnant.
Symptoms of congenital rubella syndrome are present at birth. If you get rubella while pregnant, your baby could be born with one or more symptoms of CRS, including:
To diagnose rubella, your healthcare provider will give you a physical exam and look at your rash if you have one. They might test your blood, pee (urine) or mucus from your nose or throat for signs of rubella.
Tests used to diagnose rubella include:
Advertisement
If your nose, throat or pee is tested and comes back positive, it means you’re currently infected with rubella. If your rubella blood test is positive, it means you have antibodies to rubella. Antibodies are special proteins that know how to identify specific invaders, like viruses and bacteria.
If you test positive when you’re not sick, having antibodies means you were sick with rubella before or received a vaccination for it. You’re likely to be immune to rubella if you have antibodies to it — in other words, your immune system knows how to destroy it before you get sick.
There’s no specific medicine for treating rubella. It usually gets better on its own. You can treat symptoms at home with over-the-counter medications. Your healthcare provider may suggest quarantining away from others to reduce the spread of rubella.
Most of the time, you can manage the symptoms of rubella at home with over-the-counter medicines, like acetaminophen (also known as paracetamol or under the brand names Tylenol® or Panadol®) or cough and cold medicines. Ask your healthcare provider about the best way to treat your symptoms. Check with your pediatrician before giving medications to your child for rubella.
Advertisement
The ways to treat congenital rubella syndrome depend on its severity. Some conditions are treatable with medication or surgery. Other damage is permanent, and it’s only possible to manage the condition to improve quality of life.
Rubella usually causes mild illness and goes away on its own. Since it can be contagious for up to two weeks, you should avoid being around other people as much as possible while you have symptoms and for a week after your rash appears.
If you get rubella while pregnant, talk to your healthcare provider about how it might affect the developing fetus.
Rubella causes a rash that usually lasts about three days. Other symptoms can last a few days to a week.
Rubella can be contagious for up to a week after the rash starts. Don’t go back to work or school if you have a rash or any symptoms. Talk to your healthcare provider, employer, school or child’s school to know what you need to do to return.
The most common and serious complications of rubella are pregnancy loss (miscarriage) and congenital rubella syndrome (CRS). CRS happens in babies born to someone who had rubella while pregnant. Less common complications include:
Advertisement
Yes, rubella can cause miscarriage in a pregnant woman. It can also cause conditions like cataracts, heart disease and hearing loss in your baby from birth.
The best way to prevent rubella is vaccination with the MMR (or MMRV) vaccine. Other ways to protect yourself against rubella include:
Rubella vaccination can involve either the MMR or the MMRV vaccine.
Most children and adults over the age of 12 can get vaccinated against rubella. Some people don’t need to get the vaccine and others shouldn’t get it.
You don’t need the rubella vaccine if you:
Experts recommend against getting the rubella vaccine if you:
If you bruise or bleed easily or have a close relative who has immune system problems, ask your provider if you should get the rubella vaccination.
If you or your child have symptoms of rubella, contact your healthcare provider. If you plan on getting pregnant, talk to your provider about protecting yourself against rubella before getting pregnant.
If you’re pregnant, contact your healthcare provider or go to the nearest ER if you’re experiencing:
Some questions to ask your healthcare provider include:
Rubella, measles and chicken pox can look similar since they all come with a skin rash. But they’re all different diseases, and they happen because of different viruses.
Rubella is a rubivirus of the family Matonaviridae. Its instructions are written on RNA. It has a protective shell (capsid) and an envelope that helps it invade human cells.
Before a vaccine was widely available, most people in the U.S. got rubella. The last major rubella epidemic in the U.S. was from 1964-1965. In those years, 12.5 million people got rubella, 20,000 babies were born with CRS, 11,000 miscarriages from rubella were reported and 2,100 newborns died.
After vaccines for rubella went into widespread use (starting in 1969), cases of rubella drastically dropped in the U.S. There are now only a few cases each year. In recent years, all cases of rubella diagnosed in the U.S. were acquired when traveling or living overseas.
Rubella is often a mild illness, but it can be dangerous in pregnant women. If you’re pregnant and get rubella, your child is at high risk for organ damage and other life-threatening conditions. Getting vaccinated greatly reduces your risk of getting rubella and spreading it to others.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Have a virus, fungus or bacteria? Some of these “bugs” won’t go away on their own. Cleveland Clinic’s infectious disease experts are here to help.
