Having cancer is a life-changing event. Knowing what to expect — from diagnosis to recovery — can empower you and help you take control of your health. This is a general overview of what cancer is, what causes it, how healthcare providers treat it and how you can take care of yourself throughout your journey.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
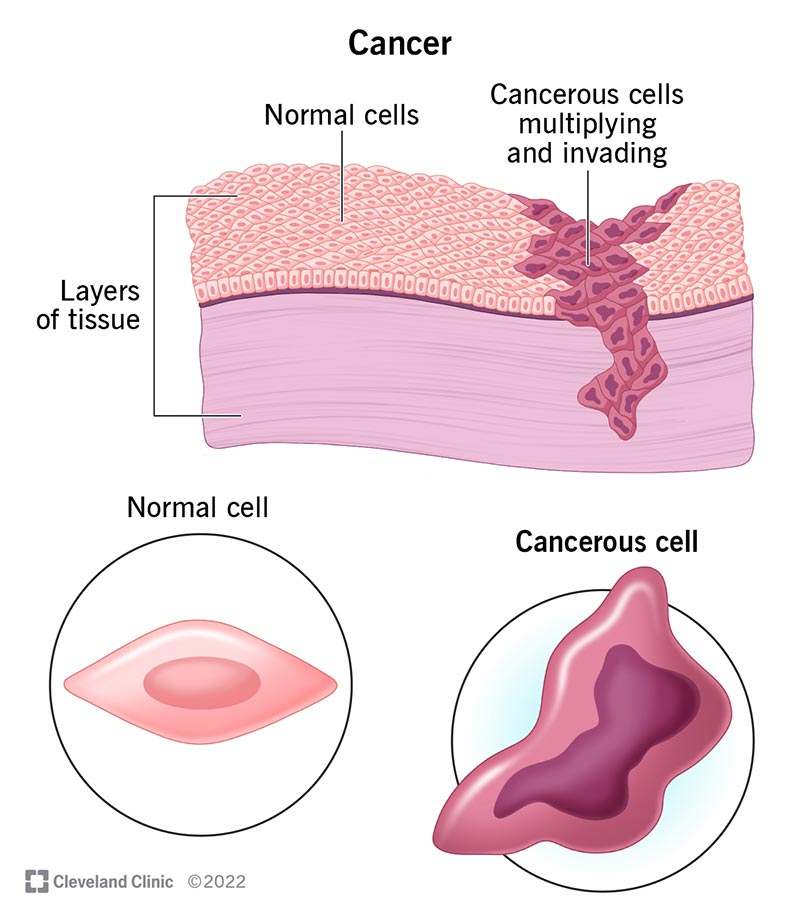
Cancer is a large group of diseases with one thing in common: They happen when normal cells become cancerous cells that multiply and spread. Your genes send instructions to your cells — like when to start and stop growing, for example. Normal cells follow these instructions, but cancer cells ignore them.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cancer is the second most common cause of death in the U.S. But fewer people are dying of cancer now than 20 years ago. Early detection and innovative treatments are curing cancer and helping people with cancer live longer.
There are over 100 types of cancer. Healthcare providers categorize them according to where they start in your body and the type of tissue they affect. There are three broad cancer classifications:
Cancer is the second most common cause of death worldwide. Researchers estimate that in 2024, over 2 million people living in the U.S. will receive a cancer diagnosis, and over 611,000 people will die from the disease.
About 1 in 4 people will develop cancer at some point during their lifetime.
Advertisement
The most common cancers in the U.S. are:
Anyone can develop cancer, but cases vary based on race and sex. According to the 2022 Annual Report on Cancer, the disease:
Symptoms of cancer vary from person to person. They depend on what type of cancer you have and how advanced it is.
General cancer symptoms may include:
In some cases, cancer may cause additional organ-specific symptoms. These may include:
This isn’t an exhaustive list. And having these symptoms doesn’t necessarily mean you have cancer.
Cancer is a complicated disease. Different types cause different symptoms. It’s also possible to have cancer for years without knowing it. Other times, it can cause obvious symptoms that get worse very quickly.
A good rule of thumb is to let a healthcare provider know any time there’s a change in your body that lasts for more than two weeks.
Cancer is a genetic disorder. But that doesn’t necessarily mean it’s inherited. It happens when genes that manage cell activity mutate (change). They create abnormal cells that divide and multiply, eventually disrupting how your body works.
These cells create cancer clusters, or tumors. Cancerous cells may break away from tumors and travel to other areas of your body through your lymphatic system or bloodstream. (Healthcare providers call this metastasis.)
For example, a tumor in your breast may spread to your lungs, making it hard for you to breathe. In some types of blood cancer, your bone marrow makes abnormal blood cells that multiply uncontrollably. Eventually, the abnormal cells crowd out normal blood cells.
According to medical researchers, inherited genetic mutations (changes you can’t control) cause about 5% to 10% of all cancers. More often, cancer occurs as an acquired genetic mutation (change). That means it happens over the course of your life. Medical researchers have identified several risk factors that increase your chance of developing cancer.
Advertisement
There isn’t one single cause for cancer. Rather, certain things can increase your chance of developing it, like:
Healthcare providers begin a cancer diagnosis by doing a complete physical examination. They’ll ask you to describe your symptoms and your family medical history. They may also need to do:
Advertisement
Healthcare providers use cancer staging systems to plan treatment and develop a prognosis or expected outcome.
Most cancers have four stages. The specific stage is determined by a few different factors, including the tumor’s size and location.
Stages I-III (1-3) (early-stage or locally advanced) usually describe cancer that has grown directly into surrounding tissue or has spread to nearby lymph nodes.
Stage IV (4) (or metastatic cancer) means that cancer cells have spread to distant areas of your body through your bloodstream or lymphatic system.
Healthcare providers may use several different treatments, sometimes combining treatments based on your situation. Common cancer treatments include:
Advertisement
Cancer treatments can cause several side effects. These side effects vary depending on which treatment you have and how your body tolerates it. If you develop side effects during your cancer treatment, let your healthcare provider know. They may be able to give you recommendations or medications that can help.
You are unique, and so is your prognosis. Your healthcare providers will base your outlook on factors like:
While there’s no single cure for cancer, some cancers respond well to treatment. Many people notice a reduction in their signs and symptoms. When this happens, healthcare providers call it remission. Partial remission is when you have fewer signs and symptoms. Complete remission is when you no longer experience symptoms at all.
Different cancers require different treatments, so outcomes vary. In general, people who receive their diagnosis and begin treatment before cancer spreads have a more positive outlook. But even if your cancer has spread beyond where it started, treatment can slow its growth, ease your symptoms, help you live longer and improve your quality of life.
Survival rates are estimates based on the experiences of large groups of people with different kinds of cancer. Like prognoses, survival rates vary based on cancer type, stage and treatment.
It’s important to remember that survival rates are only estimates. They can’t tell you how long you’ll live or how your body will respond to certain treatments. Your healthcare provider can tell you more about survival rates and what they mean for you.
You can’t always prevent cancer, especially when unavoidable risk factors cause it. But there are things you can do to lower your risk:
Self-care is an important part of living with cancer, and it looks different for everyone. Giving yourself some TLC when you need it can reduce stress and enrich your mental, emotional and spiritual well-being. The following are some self-care ideas:
Some of these things might not be your cup of tea, and that’s OK. The bottom line? Do things that bring you joy and satisfaction. Find meaningful ways to spend your time.
Tell your healthcare provider about any issues you have while you’re undergoing cancer treatment, including any treatment side effects. In many cases, your oncologist can find ways to make you more comfortable. Don’t hesitate to reach out if you’re not feeling well.
Knowledge is power. If you have cancer, you’ll want to gather as much information as you can. Here are some questions to ask your healthcare provider:
“You have cancer” may be one of the scariest things you’ll ever hear. Suddenly, everything seems uncertain. You might feel sad, alone, frustrated or angry. Maybe you’re all these things at once. Or maybe you’re totally numb. Whatever you’re feeling is valid and OK.
How will this diagnosis change me? What will my life look like now? How long do I have to spend with my loved ones? If these are the questions running through your mind, you’re not alone. The day of your diagnosis, you became a cancer survivor — a member of a global community. You’ll meet many people on this journey. Lean on them and your loved ones for support. Your healthcare providers understand the gravity of this life-changing event — and they’re here to help in whatever ways you need.
When you’re diagnosed with cancer, you want expert and compassionate care right away. At Cleveland Clinic we personalize your treatment to match your needs.

Last reviewed on 08/19/2024.
Learn more about the Health Library and our editorial process.