Prostate cancer starts in the prostate gland, part of the male reproductive system. It usually grows slowly, and many people don’t need treatment right away. But some types can spread quickly and are harder to treat. Early diagnosis improves the chances of long-term survival.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
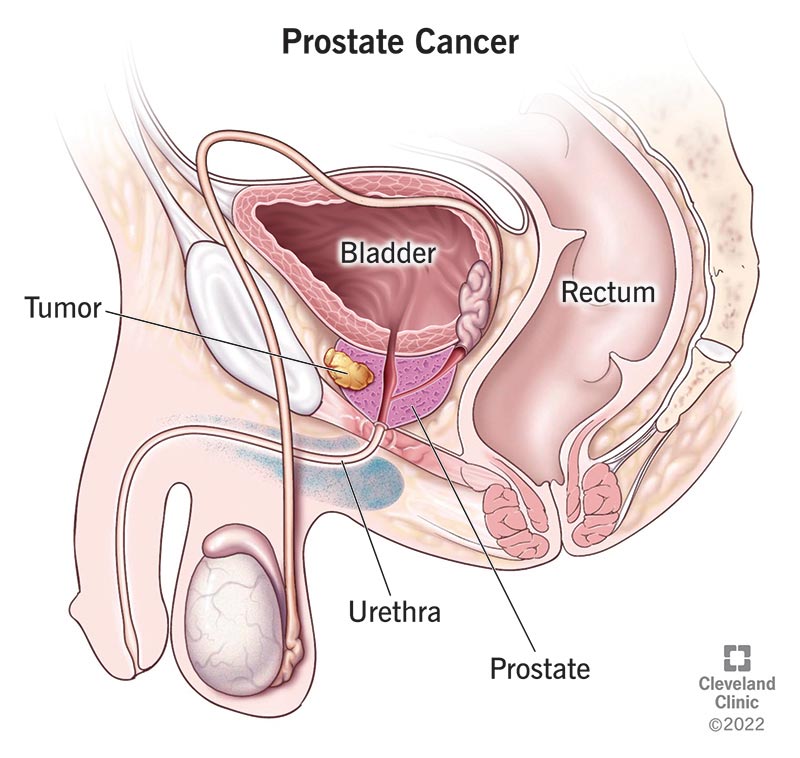
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/8634-prostate-cancer)
Prostate cancer is cancer that develops in the prostate, a small, walnut-shaped gland located below the bladder and in front of the rectum in males. This tiny gland secretes fluid that mixes with semen, keeping sperm healthy for conception and pregnancy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Prostate cancer is a serious disease. And it’s common. For every 100 males, 13 will develop prostate cancer at some point in their lives. Fortunately, most people get diagnosed before it spreads beyond their prostate glands. Treatment at this stage often eliminates the cancer. Still, approximately 35,770 people in the United States die from prostate cancer each year.
If you’re diagnosed with prostate cancer, it’s most likely an adenocarcinoma. Adenocarcinomas start in the cells of glands that secrete fluid, like your prostate. Rarely, prostate cancer forms from other types of cells.
Less common types of prostate cancers include:
Early-stage prostate cancer rarely causes symptoms. But as prostate cancer progresses, you may start to notice changes. Contact your healthcare provider if you have any of these symptoms of prostate cancer:
Advertisement
Experts aren’t sure what causes cells in your prostate to become cancer cells. As with cancer in general, prostate cancer forms when cells divide faster than usual. While normal cells eventually die, cancer cells don’t. Instead, they multiply and grow into a lump called a tumor. As the cells continue to multiply, parts of the tumor can break off and spread to other parts of your body (metastasize).
Luckily, prostate cancer usually grows slowly. Most tumors are diagnosed before the cancer has spread beyond your prostate. Prostate cancer is highly treatable at this stage.
The most common risk factors for prostate cancer include:
Some studies have identified other prostate cancer risk factors, but the evidence is mixed. Other potential risk factors include:
Doctors use screening tests, physical exams, scans and, sometimes, a biopsy to diagnose prostate cancer. Most people start screening at age 55, or earlier if they’re at a higher risk. Screening usually stops after age 70. If the results show something unusual, you may need more tests. But if your doctor thinks the tumor is slow-growing and not likely to cause problems, they may wait before doing more tests. Faster-growing cancers or those that have spread outside the prostate usually need a biopsy to confirm the diagnosis.
Screening tests can show whether you have signs of prostate cancer that require more testing:
Advertisement
Healthcare providers use the Gleason score and cancer staging to determine how serious the cancer is and the types of treatments you need.
The Gleason score allows your provider to rate how abnormal your cancer cells are. The more abnormal cells you have, the higher your Gleason score. The Gleason score allows your provider to determine the grade of your cancer, or its potential to be aggressive.
Cancer staging allows your provider to determine how advanced your cancer is, or how much it’s spread. Cancer may be in your prostate gland only (local), invading nearby structures (regional) or spreading to other organs (metastasized). Prostate cancer most commonly spreads to your bones and lymph nodes. It can also develop in your liver, brain, lungs and other organs.
Your treatment depends on multiple factors, including your overall condition, if the cancer’s spread and how fast it’s spreading. Depending on your treatments, you may work with various healthcare providers, including urologists, radiation oncologists and medical oncologists. Most prostate cancers diagnosed in the early stages can be cured with treatment.
Surveillance
If your cancer is slow-growing and hasn’t spread, your doctor may monitor it instead of treating it right away.
Advertisement
Surgery
A radical prostatectomy removes a diseased prostate gland. It can often successfully eliminate prostate cancers that haven’t spread. Your provider can recommend the best removal method if they believe you’d benefit from this surgery.
Radiation therapy
You may receive radiation therapy as a standalone treatment for prostate cancer or in combination with other treatments. Radiation can also provide symptom relief.
Advertisement
Systemic therapies
If cancer spreads outside your prostate, your oncologist may recommend systemic treatments. These therapies travel through your body to destroy cancer cells or stop them from growing.
Focal therapy
Focal therapy is a newer form of treatment that destroys tumors inside your prostate. Your healthcare provider may recommend this treatment if the cancer is low risk and hasn’t spread. Many of these treatments are still considered experimental.
Potential side effects include:
Let your cancer care team know if you have side effects. Often, they can recommend medicines and procedures that can help.
If you have prostate cancer, you may want to ask your healthcare provider:
You have an excellent outlook when prostate cancer is found early. Almost everyone — 99% — diagnosed before it spreads lives at least five years after diagnosis. In many cases, treatment can eliminate cancers that stay in the prostate. Survival rates aren’t as good if the cancer spreads — 32% of people with metastatic prostate cancer are alive five years after diagnosis.
Learning you have prostate cancer can bring up a lot of emotions — and questions. The good news is that when it’s found early, prostate cancer is often highly treatable. Many people go on to live full, cancer-free lives for years after treatment. Still, some cases can be more aggressive and spread more quickly. Your cancer care team will help you understand your options and guide you through each decision — from screening to treatment — with support that’s tailored to your needs and goals.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A prostate cancer diagnosis can change your life. At Cleveland Clinic, we can help you feel like yourself again with expert treatment and support.
