Carcinoma is the most common type of cancer, accounting for 80% to 90% of all cancer diagnoses. Carcinoma forms in epithelial tissue which is tissue that lines your organs, internal passageways in your body and your skin. Carcinoma appears as tumors that may form on your skin or in your lungs, breasts, prostate, colon, kidneys, pancreas, etc.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
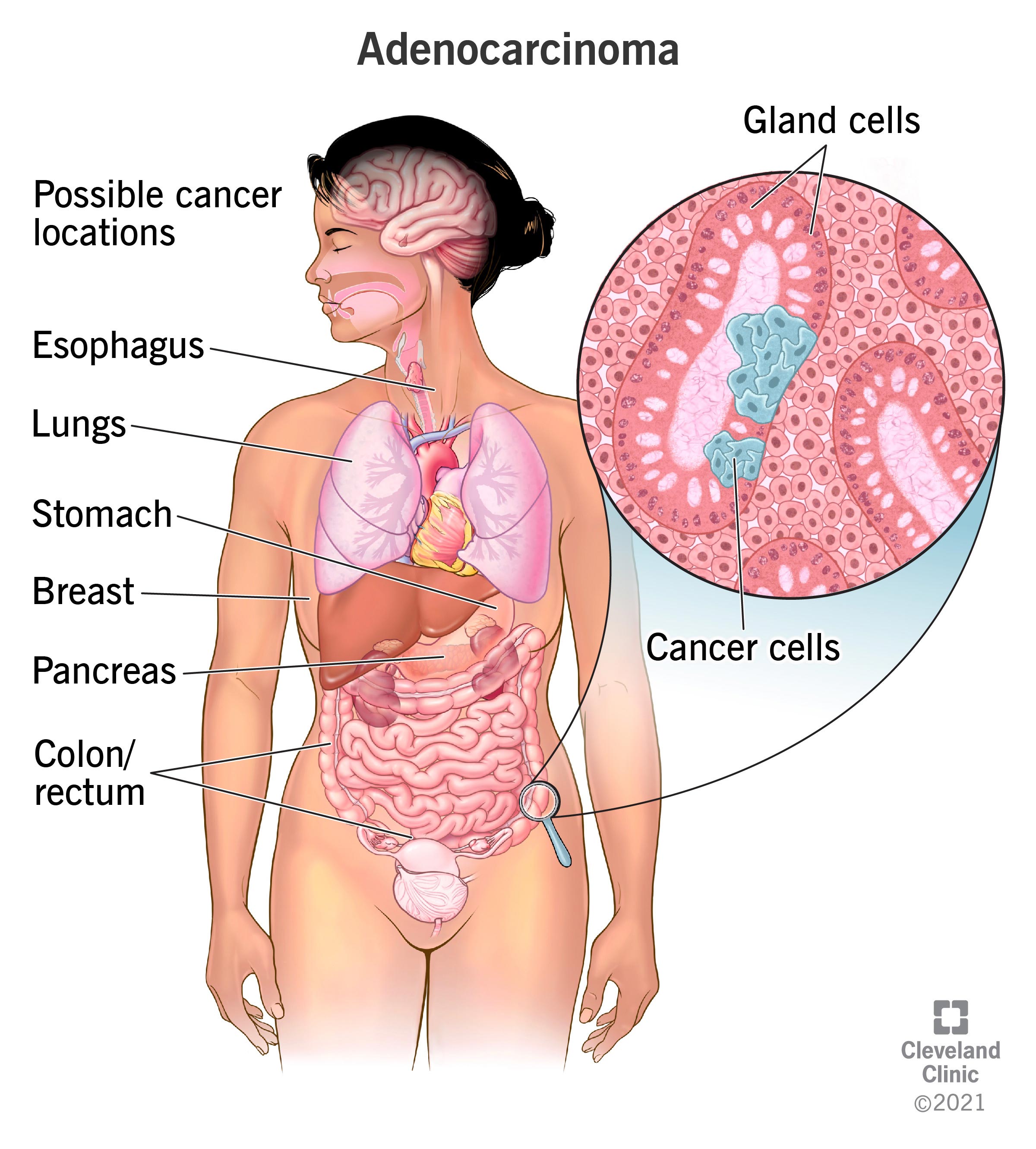
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/23180-carcinoma)
Carcinoma is cancer that forms in epithelial tissue. Epithelial tissue lines most of your organs, the internal passageways in your body (like your esophagus), and your skin. Most cancers affecting your skin, breasts, kidney, liver, lungs, pancreas, prostate gland, head and neck are carcinomas.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Most people think of cancer in terms of where it forms (breast cancer, colon cancer, etc.), but this is just one way to distinguish one type of cancer from another. Scientists also classify cancers based on the types of tissue where cancer cells start growing.
Cancer classifications by tissue type include:
As carcinoma cells grow and multiply, they form solid masses called tumors. Cancer cells can break away from tumors and spread to other parts of your body (metastasize). Labels for carcinoma describe how much it has spread.
There are multiple cancers classified as carcinomas. The most common carcinoma types include the following:
Advertisement
Certain demographic factors may influence your likelihood of developing carcinoma.
Carcinoma is the most common form of cancer, making up 80% to 90% of cancer diagnoses.
Carcinoma, like all cancer, begins when a genetic mutation (change) transforms a normal, healthy cell into a cancer cell. That cancer cell keeps multiplying and making more cancer cells. Untreated, the cancer cells can invade nearby healthy tissue. Eventually, the cancer cells may travel through your bloodstream or lymphatic system to invade other parts of your body (metastasize).
Scientists don't know what causes the mutation that leads to cancer, but certain factors may increase your risk.
Advertisement
Risk factors vary depending on the specific type of carcinoma.
Risk factors for adenocarcinoma are significantly varied since these types of carcinoma may present in multiple organs, including your breast, prostate, pancreas, esophagus, colon/rectum, stomach, lungs, etc. Common risk factors include:
Your provider will conduct a thorough medical history and review your family medical history to identify factors that may increase your carcinoma risk. They will ask you about your symptoms. Your provider may recommend any of the following tests or procedures if they suspect you have carcinoma.
Advertisement
Advertisement
An essential part of diagnosis involves staging cancer. Staging allows your provider to document a tumor's size, lymph node spread or spread to other parts of your body. It also provides important information about its spread.
Carcinoma treatment depends on various factors, including your overall health, stage of the tumor, details of the biopsy report such as pathology, your age and what you want out of treatment. Your provider will discuss a care plan with you that matches your unique situation.
Depending on your diagnosis, treatment may be curative, palliative or both. The goal of curative treatment is remission. Complete cancer remission means that the signs and symptoms of the cancer are no longer present. Palliative care can help you manage cancer symptoms. It can also empower you to feel more comfortable and confident with care decisions as you navigate life with a cancer diagnosis.
Carcinoma's seriousness depends on the type of carcinoma, where it's located, when you were diagnosed, and how much it's spread, among other factors. Generally, metastatic carcinoma is more serious than carcinoma in situ. Slow-growing carcinoma like basal cell carcinoma tends to be less serious than fast-growing cancers, like Merkel cell carcinoma.
Still, your outlook depends on specific factors that only you and your provider know. Ask your provider about what your diagnosis and health mean for your prognosis.
First, it helps to know potential risk factors and communicate them with your provider. For example, suppose a close family member had breast cancer. In that case, your provider may recommend early screenings or more frequent breast exams. They may recommend genetic testing to see if you have gene mutations that may indicate a greater risk of carcinoma.
Certain lifestyle behaviors can reduce your risk of some carcinoma types:
If you’ve been diagnosed with carcinoma, it may be helpful to ask your healthcare provider the following questions:
Carcinoma is a type of cancer that forms in epithelial tissue. Other types of cancer form elsewhere, such as in connective tissue (sarcoma), bone marrow (leukemia), etc. Most cancer diagnoses are carcinoma.
Carcinoma cells can be treated early before multiplying and becoming a mass (tumor). Untreated, however, carcinoma usually forms a tumor. Carcinoma is different from other cancers that aren't often associated with tumors, like leukemia.
Some forms of carcinoma can be cured with early detection and early treatment. For instance, basal cell carcinoma (BCC) has a 100% five-year survival rate. This means that people with BCC are just as likely to be alive five years after diagnosis as someone without a BCC diagnosis. Squamous cell carcinoma has a similar five-year survival rate of 95%.
Talk to your provider about your prognosis based on your specific carcinoma.
Many people who learn they have carcinoma rightfully wonder, is it serious? The honest answer can feel frustrating. It depends. Having carcinoma means that cancer has formed in a specific type of tissue. Other factors, like the size of the tumor, where it's located in your body, whether it's spread, etc., may provide better information about what's involved in your treatment plan. These details also inform the likelihood of getting rid of cancer over the long term. Ask your provider about how the characteristics of your carcinoma and your health influence your chance of remission.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic treats all types of carcinoma. We offer the latest options for diagnosis and personalized treatment — focusing on you and your needs.
