Hyperglycemia (high blood sugar) is common in people who have diabetes. If it’s left untreated, chronic hyperglycemia can lead to diabetes complications, such as nerve damage, eye disease and kidney damage.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hyperglycemia happens when there’s too much sugar (glucose) in your blood. It’s also called high blood sugar or high blood glucose. This happens when your body has too little insulin (a hormone) or if your body can’t use insulin properly (insulin resistance).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hyperglycemia usually means you have diabetes, and people with diabetes can experience hyperglycemia episodes frequently.
If you have hyperglycemia that’s untreated for long periods of time, it can damage your nerves, blood vessels, tissues and organs.
Severe hyperglycemia can also lead to an acute (sudden and severe) life-threatening complication called diabetes-related ketoacidosis (DKA), especially in people with diabetes who take insulin or people with undiagnosed Type 1 diabetes. This requires immediate medical treatment.
For people undiagnosed with diabetes, hyperglycemia is blood glucose greater than 125 mg/dL (milligrams per deciliter) while fasting (not eating for at least eight hours).
A person has prediabetes if their fasting blood glucose is 100 mg/dL to 125 mg/dL.
A person with a fasting blood glucose greater than 125 mg/dL on more than one occasion usually receives a diabetes diagnosis — typically Type 2 diabetes. People with Type 1 diabetes usually have very high blood sugar (above 250 mg/dL) upon diagnosis.
For a person with diabetes, hyperglycemia is usually considered to be a blood glucose level greater than 180 mg/dL one to two hours after eating. But this can vary depending on what your target blood sugar goals are.
Advertisement
Glucose (sugar) mainly comes from carbohydrates in the food and drinks you consume. It’s your body’s main source of energy. Your blood carries glucose to all of your body’s cells to use for energy.
If you don’t have diabetes, several bodily processes naturally help keep your blood glucose in a healthy range. Insulin, a hormone your pancreas makes, is the most significant contributor to maintaining healthy blood sugar.
High blood sugar most often happens due to a lack of insulin or insulin resistance. This leads to diabetes. People who have diabetes must use medication, like oral diabetes medications or synthetic insulin, and/or lifestyle changes to help keep their blood sugar levels in range.
Hyperglycemia and diabetes are very common — about 1 in 10 people in the United States has diabetes. Hyperglycemia episodes are also very common in people with diabetes.
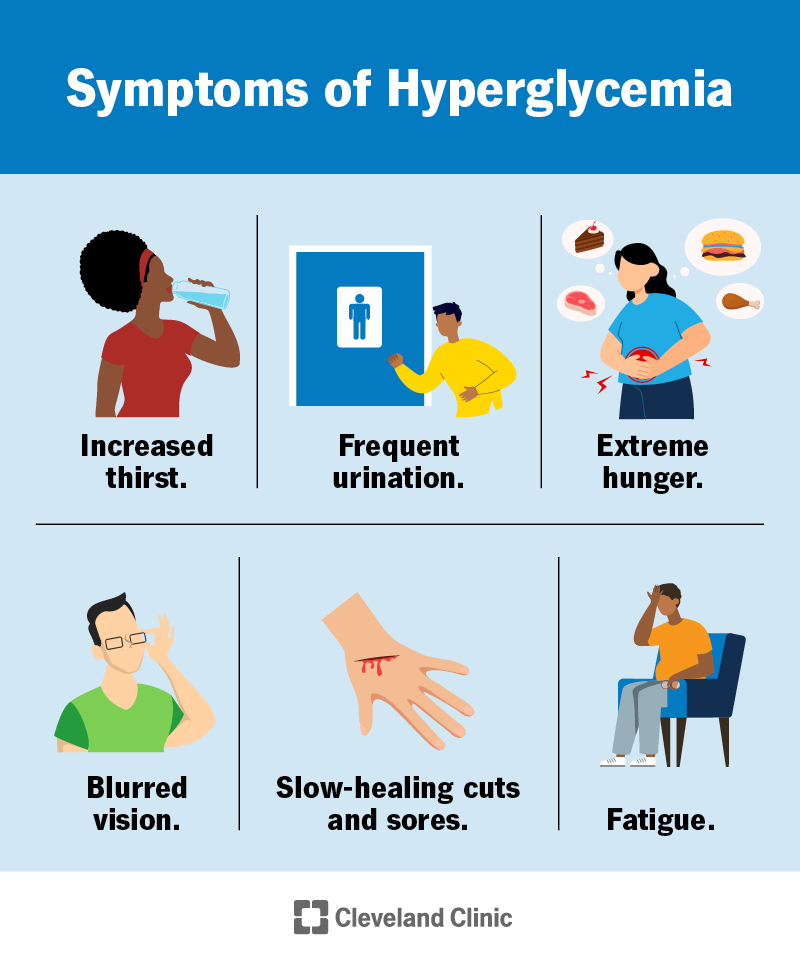
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9815-hyperglycemia)
Early symptoms of hyperglycemia include:
Symptoms of long-term hyperglycemia include:
You should see your healthcare provider if you or your child is experiencing these symptoms.
The glucose level at which people with diabetes start to experience symptoms varies. Many people don’t experience symptoms until their blood sugar is 250 mg/dL or higher. People who haven’t yet been diagnosed with diabetes typically experience these symptoms at lower levels.
It’s especially important to know the early signs of hyperglycemia and to monitor your blood sugar regularly if you take insulin or other medications for diabetes. If hyperglycemia is left untreated, it can develop into diabetes-related ketoacidosis (DKA), in which a lack of insulin and a high amount of ketones cause your blood to become acidic. DKA can also affect people who have undiagnosed Type 1 diabetes. This condition is an emergency situation that can lead to coma or death.
Symptoms of ketoacidosis include:
Seek immediate medical help if you or your child is experiencing symptoms of DKA.
Hyperglycemia most often results from a lack of insulin. This can happen due to insulin resistance and/or issues with your pancreas — the organ that makes insulin.
Advertisement
Other hormones can contribute to the development of hyperglycemia as well. Excess cortisol (the “stress hormone”) or growth hormone, for example, can lead to high blood sugar:
A common cause of hyperglycemia is insulin resistance. Insulin resistance, also known as impaired insulin sensitivity, happens when cells in your muscles, fat and liver don’t respond as they should to insulin.
When your cells don’t properly respond to insulin, your body requires more and more insulin to regulate your blood sugar. If your body is unable to produce enough insulin (or you don’t inject enough insulin), it results in hyperglycemia.
Insulin resistance is the main cause of Type 2 diabetes, but anyone can experience it, including people without diabetes and people with other types of diabetes. It can be temporary or chronic.
Common causes of insulin resistance include:
Advertisement
Certain hormonal conditions can lead to insulin resistance, such as:
Certain inherited genetic conditions are also associated with insulin resistance, including:
Damage to your pancreas can lead to a lack of insulin production and hyperglycemia. Pancreatic conditions that can cause hyperglycemia and diabetes include:
Advertisement
Certain situations can temporarily increase your blood sugar levels and cause hyperglycemia in people with and without diabetes.
Physical stress, such as from an illness, surgery or injury, can temporarily raise your blood sugar. Acute emotional stress, such as experiencing trauma or work-related stress, can increase your blood sugar as well. This is because your body releases cortisol and/or epinephrine (adrenaline).
Several factors can contribute to hyperglycemia in people with diabetes. It can develop if things like food and diabetes medications are out of balance.
Common situations that can lead to hyperglycemia for people with diabetes include:
Prolonged (chronic) hyperglycemia over the years can damage blood vessels and tissues in your body. This can lead to a variety of complications, including the following:
It’s important to remember that other factors can contribute to the development of diabetes complications, such as genetics and how long you’ve had diabetes.
Acute (sudden and severe) hyperglycemia can lead to DKA, which is life-threatening.
Healthcare providers order bloodwork to screen for hyperglycemia and diagnose diabetes. These tests may include:
People with diabetes use at-home blood sugar testing (using a glucose meter) to monitor their blood sugar and check for hyperglycemia. If you use continuous glucose monitoring (CGM), your device may alert you to high blood sugar. As this technology can sometimes be inaccurate, it’s important to check your blood sugar with a glucose meter if the CGM reading doesn’t match how you feel.
If you take insulin to manage diabetes, injected insulin is the main way to treat hyperglycemia episodes. Everyone requires different insulin doses. You and your healthcare provider will determine which dose is best for you to treat and prevent high blood sugar. Dietary changes and exercise plans can also help manage your blood sugar to prevent hyperglycemia.
For people with Type 2 diabetes who don’t require injected insulin, lifestyle changes, such as dietary changes and exercise, as well as oral diabetes medications, can help manage hyperglycemia. You and your provider will determine the plan that’s best for you.
The prognosis (outlook) of people with hyperglycemia varies based on how well they manage their diabetes overall.
Several factors affect how well a person can manage diabetes, including:
Chronic hyperglycemia can cause severe complications, and the complications are usually irreversible. Several studies have shown that untreated chronic hyperglycemia shortens lifespans and worsens the quality of life.
It’s important to know that you can live a healthy life with diabetes. The following are key to a better prognosis:
Studies have shown that people with diabetes may be able to reduce the risk of complications by consistently keeping their A1C levels below 7%.
Unfortunately, it can be difficult to totally prevent high blood sugar when you have diabetes. But you can adjust your diabetes management plan to try to reduce the number of hyperglycemia episodes you experience.
It’s easiest to do this when you and your healthcare provider understand what causes your blood sugar to rise. Give your healthcare provider as much information as possible about any high blood sugar episodes. Fixing the problem may be as simple as changing the times you take medication, eat and exercise.
The following steps can help prevent high blood sugar:
If you have diabetes and are experiencing frequent high blood sugar episodes, talk to your provider who helps you manage diabetes. They can help you adjust your management plan, which may include changes to your medication regimen, meal plans or exercise routine.
If you’re experiencing symptoms of DKA, such as high blood sugar with vomiting and extreme thirst, go to the emergency room. DKA requires immediate medical treatment.
Hyperglycemia is high blood sugar. “Hyper-” means “above” or “beyond.” Hypoglycemia is low blood sugar. “Hypo-” means “below.”
Hyperglycemia is quite common in people with diabetes. Monitoring your blood sugar regularly and seeing your diabetes healthcare provider regularly can help you properly manage diabetes and hyperglycemia. It’s important to remember that high blood sugar doesn’t have to be chronic. Know that there are steps you can take to prevent it. If you’re feeling overwhelmed with diabetes management, talk to your healthcare provider. Together, you can formulate a plan to get closer to your management goals.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
