A coma is a deep unconscious state where you can’t wake up or respond, even to pain or loud sounds. Head injuries, strokes, infections or overdoses, among other things, can cause it. A coma is a medical emergency. Treatment focuses on finding and managing the cause to prevent lasting damage.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A coma happens when you’re unconscious, unresponsive and unaware of what’s going on around you. You can’t wake up, think, talk, respond to a conversation or react to the feeling of pain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are several possible causes, like brain injuries, stroke, complications from substance use or infections, among others.
A coma is a medical emergency that requires immediate attention. It’s a common reason people end up in emergency rooms.
Comas typically don’t last longer than a couple of weeks. Severe brain injuries may lead to a persistent vegetative state or possible brain death. Delaying treatment may lead to serious complications or life-threatening outcomes.
The types vary based on the cause:
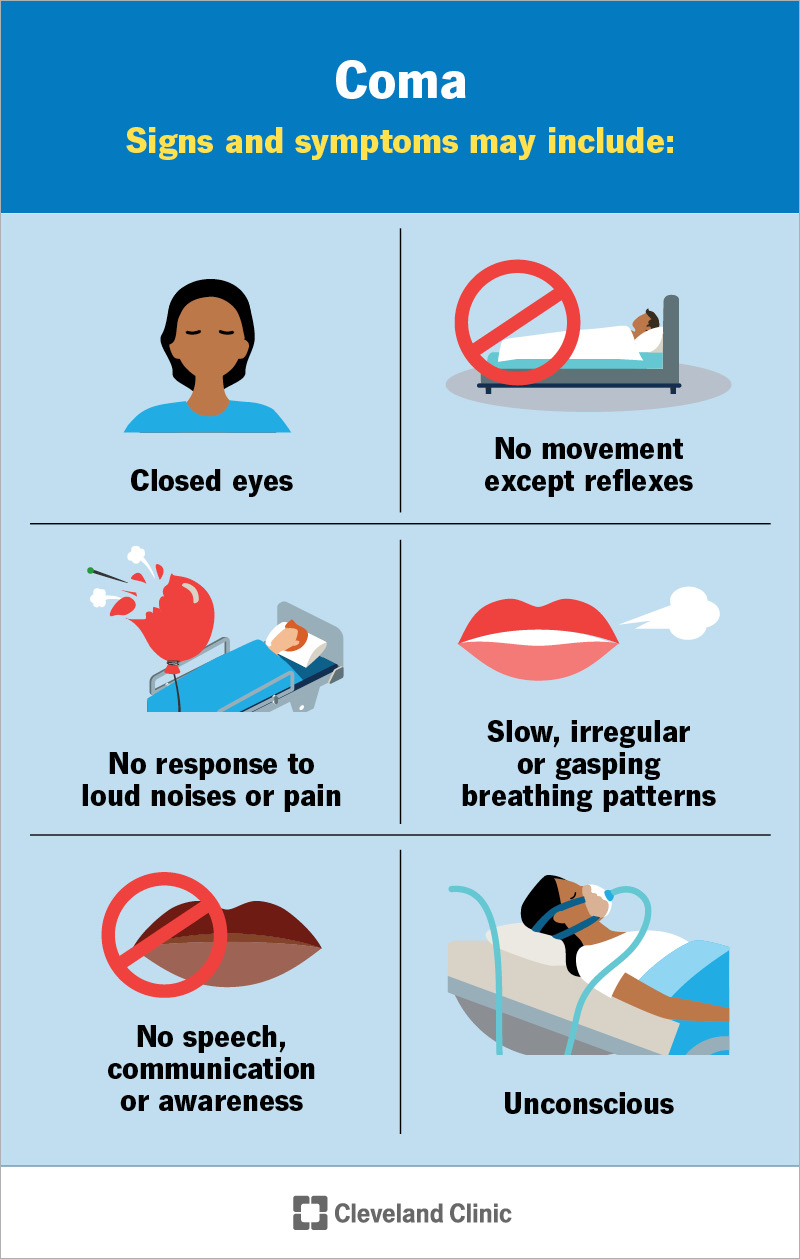
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/coma)
Signs and symptoms may include:
These can vary from person to person. While many signs are common, some people may move differently. Comas also range in severity.
Advertisement
A coma occurs when something disrupts how your brain works. This could happen to your:
Common causes may include:
Anyone can fall into a coma. But you might be more at risk if you have:
Your risk also goes up if you skip a helmet during activities like biking, motorcycling or contact sports, or if you don’t wear a seatbelt in the car.
If you’re in a coma, you can’t care for yourself. You’ll need around-the-clock medical support. You might need tube feeding, a urinary catheter to collect pee and a ventilator to help you breathe.
Complications from being in a coma or receiving coma-related care may include:
If you’re unconscious, providers will immediately check your vitals, which include your breathing, heart rate and blood pressure. They may offer immediate treatment, like sugar for low blood sugar or opioid reversal medication if they suspect an overdose.
Your providers will perform a physical and neurological exam. They’ll use the Glasgow Coma Scale to identify the severity. The GCS measures three categories:
A total score ranges from 3 to 15. A score of 15 means fully alert, and 8 or below usually indicates a coma.
Tests help confirm a diagnosis and find the cause. Common tests include:
Your provider may need other tests based on the situation. A healthcare provider can explain what’s being done and why.
Severe brain injuries can lead to disorders of consciousness. This describes how awake and aware a person is. A provider might use these terms to describe a diagnosis better:
Advertisement
Treatment may include:
Your care team will watch how your body responds. They may use the Glasgow Coma Scale to check your progress.
As you recover, your body and brain need time to heal. You may not be able to talk or move right away. But even small signs of awareness, like following something with your eyes, are important. Healthcare providers use the Coma Recovery Scale to track these signs.
Advertisement
The scale measures:
This scale helps your care team see how you’re progressing. It can help them choose the right treatments to support your recovery.
Being in a coma means you’re not conscious, so you don’t know you’re in a coma. You don’t show any signs of awareness of the world around you, and you can’t react to your environment or your body’s needs. Depending on the depth of the coma, you may still have some reflex responses. But these vary from case to case.
A coma can be very brief and last only a few minutes, or it can last as long as one to two weeks. Unfortunately, death is a possible complication. This is more likely with severe injuries, serious illness or delayed medical care.
Most comas don’t last more than a few weeks. People often either wake up or shift into a different state of reduced consciousness.
The outcome depends on many factors. A healthcare provider familiar with the case is the best person to explain what to expect.
If you’re ever in a coma, loved ones will have to make medical decisions for you. Talking with them ahead of time about your wishes and putting those wishes in writing can help ensure your choices are respected. Legal documents like advance directives can guide your care if you’re unable to decide for yourself.
Advertisement
It’s possible. Some people in a coma can hear what’s happening around them and even remember parts of it later. But this varies a lot and is hard to predict. A healthcare provider can help you understand what this might mean for you or your loved one’s recovery.
A coma can feel especially frightening, not just because it’s serious, but because it often comes with so many unknowns. When someone you love is unresponsive, it’s natural to feel scared, helpless and full of questions.
What’s important to know is that no two comas are the same. They can have many causes and lead to different outcomes. Some people wake up quickly, while others take longer or need more support. Care teams act fast to protect the brain and give each person the best chance at recovery.
If you or a loved one has a condition that raises the risk of coma, staying on top of treatment matters. And if you’ve thought about making your healthcare wishes known, now is a good time to complete an advance directive.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
