Atherosclerosis is a hardening of your arteries from plaque building up gradually inside them. Plaque consists of fat, cholesterol and other substances. This plaque buildup limits blood flow. You may not have symptoms of atherosclerosis until you have complications like a heart attack or stroke.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
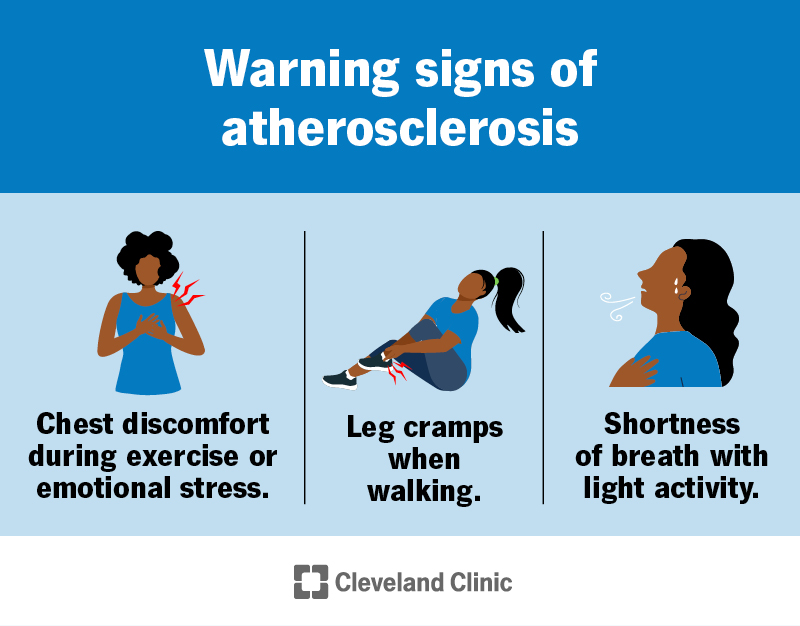
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16753-atherosclerosis)
Atherosclerosis is the gradual buildup of plaque in the walls of your arteries. Arteries are blood vessels that carry oxygen-rich blood to organs and tissues throughout your body. Plaque (atheroma) is a sticky substance made of fat, cholesterol, calcium and other substances.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As plaque builds up, your artery wall grows thicker and harder. This “hardening of the arteries” is usually a silent process in the early stages. You may not notice symptoms for a long time. But eventually, as the plaque grows, the opening (lumen) of your artery narrows, leaving less room for blood to flow. This means less blood can reach your organs and tissues. Plus, the constant force of blood flow can lead to plaque erosion or rupture, causing a blood clot to form.
A narrowed artery is like a highway reduced to one lane. But a blood clot is like a barricade in the middle of the road. It blocks blood flow to certain organs or tissues the artery normally feeds. The effects on your body depend on where the blood clot forms. For example, blockages in a coronary artery deprive your heart of oxygen-rich blood, leading to a heart attack.
Atherosclerosis is very common. The complications of plaque buildup (including heart attacks and strokes) are the leading cause of death worldwide.
In America, about half of people age 45 to 84 have atherosclerosis but aren’t aware of it, according to the U.S. National Institutes of Health.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_wsnqeafb/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn more about the signs of atherosclerosis.
Atherosclerosis symptoms often don’t start until an artery is very narrow or blocked. Many people don’t know they have plaque buildup until they have a medical emergency like a heart attack or stroke.
Advertisement
You may notice symptoms of atherosclerosis if your artery is more than 70% blocked. You can have symptoms in different parts of your body, depending on the location of the blockage. Affected locations may include:
Heart
Coronary artery disease (CAD, which can lead to a heart attack) happens in the arteries that supply blood to your heart.
You may experience:
Digestive system
Mesenteric ischemia happens when you don’t have enough blood flow in parts of your digestive system. You may experience:
Legs and feet
Peripheral artery disease (PAD) refers to poor blood flow in the arteries in your limbs.
You may experience:
Kidneys
With renal artery stenosis (narrowing of the arteries that take blood to your kidneys), you may experience:
Brain
With carotid artery disease, the first symptoms are usually a transient ischemic attack (TIA) or stroke.
You may experience:
Researchers believe atherosclerosis causes may include:
These factors can damage your artery’s inner lining (endothelium). This causes atherosclerosis to begin. The damage usually occurs slowly and over time.
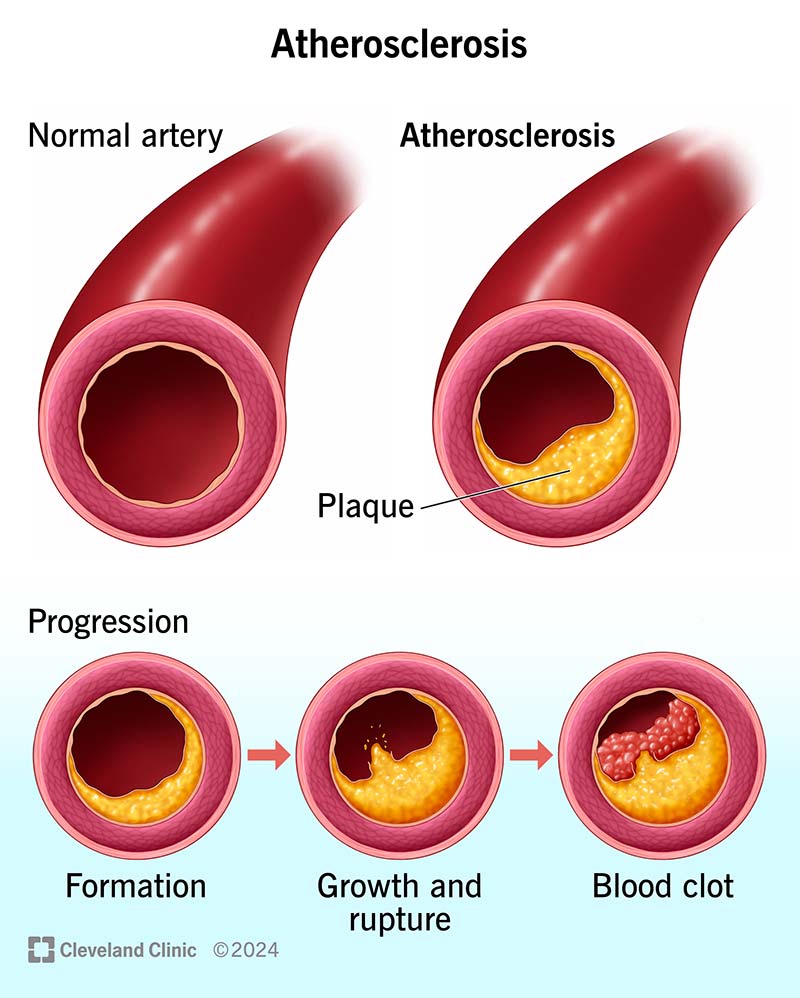
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16753-atherosclerosis-illustration)
Atherosclerosis involves gradual plaque buildup inside your artery.
The stages of atherosclerosis happen over many years and include:
Advertisement
There are many risk factors for atherosclerosis. You may be able to change some of these risk factors, but not others (like age).
Risk factors include:
Atherosclerosis interferes with the normal workings of your cardiovascular system. It can limit or block blood flow to various parts of your body, including your heart and brain. Possible complications of reduced blood flow include:
Advertisement
Early diagnosis and treatment of atherosclerosis can help you avoid or delay complications.
To diagnose atherosclerosis or calculate your risk for developing it, a healthcare provider will:
Your healthcare provider may order additional tests to diagnose atherosclerosis and plan treatment. These tests include:
Advertisement
Atherosclerosis treatment includes lifestyle changes, medications, procedures or surgeries. Depending on the location of your atherosclerosis, you may see a cardiologist (heart), nephrologist (kidneys), neurologist (brain and spine) or vascular surgeon (blood vessels).
Your healthcare providers will develop a plan based on your needs. Common treatment goals include:
Lifestyle changes may lower your risk of complications. Your provider will create a plan specific to your needs. General tips include:
Medications target risk factors for plaque buildup and may help slow the progression of atherosclerosis. Your provider may prescribe medications that lower your blood pressure or cholesterol, manage your blood sugar levels and prevent blood clots.
Various minimally invasive procedures and complex surgeries can help people with severe blockages or a high risk of complications. Common treatment options include:
Early diagnosis and treatment can help people with atherosclerosis keep doing the activities they like to do. But the disease can cause medical emergencies and even be fatal. That’s why knowing your risks and working with your healthcare provider to lower them is important.
You may not be able to prevent atherosclerosis. But you can reduce your risk and lessen the effects of the disease. Here are some steps you can take:
It’s essential to work closely with your healthcare provider. They’ll keep a close eye on your condition and tell you how often you should come in for appointments. Go to all of your appointments and be an active partner in your care. Tell your provider right away about any new or changing symptoms. Early treatment can lower your risk of life-threatening complications.
Also, take care of your mental health. It’s normal to feel anxious about what the future could bring. You may also feel overwhelmed by the need to make lifestyle changes. But those feelings shouldn’t prevent you from enjoying life. Some tips for managing your thoughts and worries include:
Call 911 or your local emergency number right away if you or someone near you has symptoms of a heart attack, stroke or TIA. These are medical emergencies that require immediate care.
Questions to ask your healthcare provider may include:
Atherosclerosis is a common condition that many people are facing. But your healthcare provider is ready to help you manage your condition so you can live your best life. In your yearly checkup, they’ll evaluate your risk for atherosclerosis and explain what you can do to lower it. Don’t be afraid to ask for help in carrying out your provider’s instructions. They can suggest resources for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you need treatment for coronary artery disease, you want expert care. At Cleveland Clinic, we’ll create a treatment plan that’s personalized to you.
