An exercise stress test helps determine how well your heart responds during times when it's working its hardest. It typically involves walking on a treadmill or pedaling on a stationary bike while hooked up to an EKG to monitor your heart’s activity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
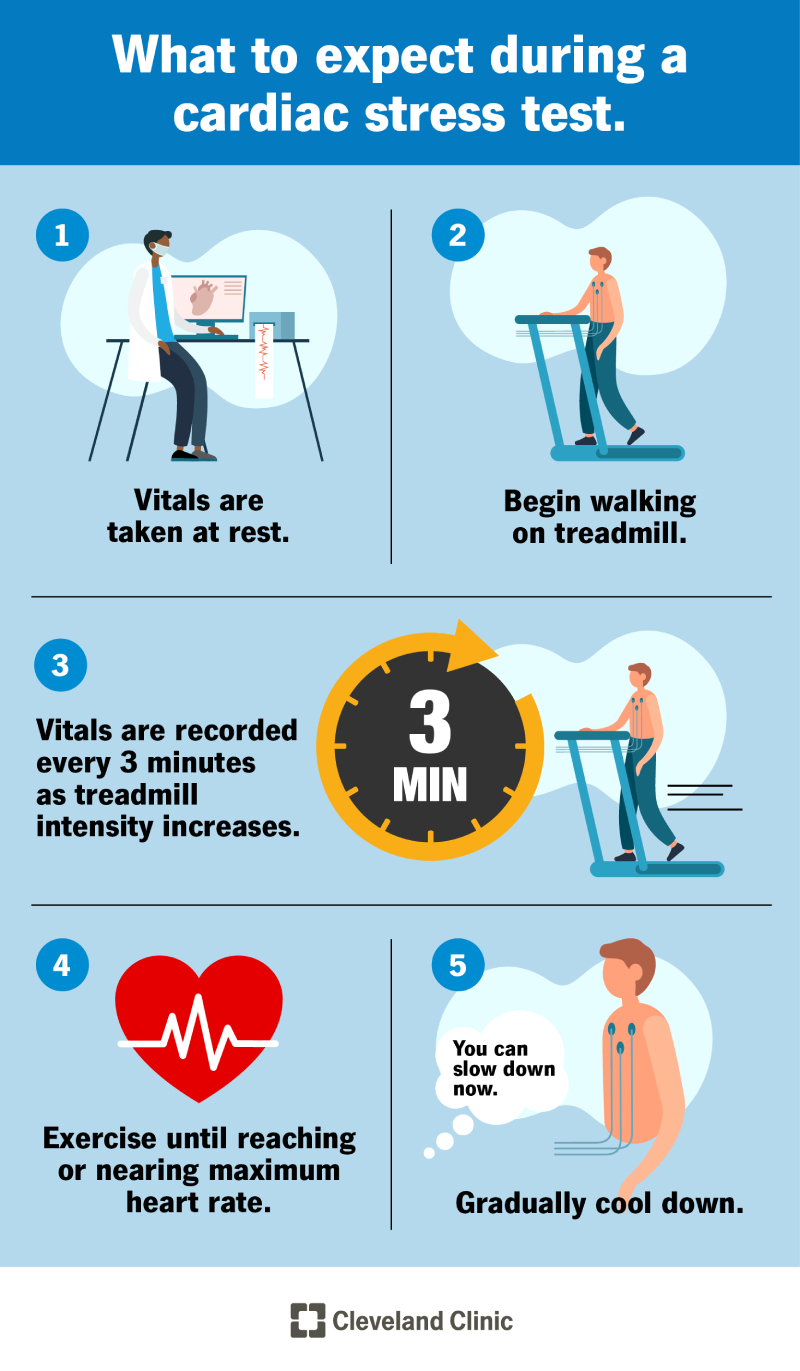
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16984-exercise-stress-test)
A stress test is a very commonly performed test to learn:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This makes it easier to identify and evaluate certain heart issues, such as:
Cardiac stress tests help healthcare providers determine whether you need additional — often more invasive — testing to confirm a diagnosis or if treatment might lower your heart attack risk and make you feel better.
A heart stress test starts by making your heart pump harder and faster. For many people, this includes walking on a treadmill or riding a stationary bicycle. That’s why the test is often called an exercise stress test.
Healthcare providers assess your response to the increased workload by measuring:
Advertisement
You may need this test to detect heart problems like:
People with high-risk occupations (like pilots or professional athletes) may also need stress tests.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_yddzwrse/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn what a cardiac stress test is, why it’s done and how it helps doctors detect hidden heart problems.
This test may be right for you if you have symptoms of heart disease, like:
Stress tests are also for people with a heart disease diagnosis who:
Providers may also do stress tests in people without known heart disease or symptoms to assess their risk for heart disease and heart attacks, especially if they have other risk factors like diabetes, high blood pressure, high cholesterol or a family history of premature heart disease.
There are many methods for assessing heart function while it’s hard at work. All cardiac stress tests involve checking your heart rate, blood pressure, oxygen levels and electrical activity. But there are some differences.
Stress test types include:
This is the most common and basic heart stress test. It involves walking on a treadmill or riding a stationary bicycle. A well-trained exercise physiologist usually tailors the speed and elevation of the treadmill to your ability to walk and your overall fitness.
If you can’t exercise, you receive medications that make your heart pump harder and faster or dilate the artery supplying blood to your heart (coronary arteries). An electrocardiogram (EKG) captures your heart’s electrical activity. Exercise stress tests check for signs of coronary artery disease.
An exercise stress echocardiogram is similar to the basic stress test but provides more detail. Healthcare providers perform an echocardiogram (ultrasound of your heart) before and at peak exercise. This cardiac imaging test uses sound waves to evaluate blood flow through your heart as well as the pumping chambers of your heart (muscle) and valve functions.
You might need a stress echocardiogram if the results of your initial stress test are unclear. This study enables healthcare providers to observe blood flow through the heart’s chambers as well as the effects of exercise.
Advertisement
This advanced heart stress test uses safe levels of a radioactive substance and a cardiac imaging scan to assess heart function. A healthcare provider takes pictures of your heart before (at rest) and after you exercise. A cardiologist compares the amount of blood flow to the muscle of your heart at rest and after stress. A decrease in blood flow signal usually indicates a blockage in one or multiple arteries in your heart.
Nuclear cardiac stress tests can:
If your healthcare provider recommends cardiac rehabilitation, the program may include stress testing. Rehabilitation is a medically supervised exercise program that helps people with heart disease become more physically active.
Cardiac rehabilitation stress testing includes:
Advertisement
Cardiac stress testing isn’t for everyone. You might not need the test if you have:
The test is also not for people with heart conditions that make stress testing unsafe (contraindications). These include:
Your healthcare provider may decide not to have you undergo stress tests or repeat “routine” stress tests to help you avoid unnecessary costs and treatments. An unindicated stress test may show results that prompt healthcare providers to recommend additional testing you don’t need. Some of these tests, including a coronary angiogram, carry a higher risk of complications than stress tests.
Cardiologists consider your overall health in determining whether a heart stress test is right for you. This determination includes your:
Advertisement
Females tend to experience heart disease differently than males. This makes it challenging to detect early-stage heart disease. In general, healthcare providers tailor their stress testing and method of imaging during stress testing based on your sex and age to obtain optimal results and minimize radiation and unclear test results.
If there are no contraindications, exercise stress tests are safe. Very few people experience complications. Trained healthcare providers, typically an exercise physiologist and a cardiologist, are present during your test in the rare event that you have a complication. They assess your performance, data and symptoms throughout the tests and immediately provide emergency treatment if it’s needed. You also have the option of stopping the stress test at any time if you become anxious or uncomfortable.
If you’re undergoing a basic stress test, the exercise portion lasts about 10 to 15 minutes. Additional time is necessary for getting ready to exercise and recovering afterward.
Stress tests that include echocardiography, nuclear imaging or MRI often are longer and may require you to be in the stress lab for up to three hours.
To prepare, you should:
It’s important not to eat before your test. However, you shouldn’t skip meals, especially if you’re taking diabetes medications. Talk to your diabetes care provider if you need assistance coordinating your meals and medications for test day.
If you own a glucose monitor, bring it with you so you can check your blood sugar levels before and after the test.
Here’s what to expect during an exercise stress test:
You receive medications through a vein in your arm (intravenously). The medications simulate the effects of exercise on your heart by making it pump harder and faster. It can take up to an hour for you to start feeling the effects.
You follow the same steps as an exercise stress test. In addition, you lie down on a table before and after exercising to undergo an echocardiogram. This imaging study uses sound waves (ultrasound) to capture images of your heart pumping. It enables healthcare providers to observe the effects of exercise in more detail.
The whole test takes about an hour, but you exercise for less than 15 minutes.
For a nuclear stress test, you receive an injection of a radioactive substance. There is enough substance to show small details of heart activity during a sophisticated imaging study (SPECT or PET scan). The level of radiation is low and isn’t associated with any known, immediate side effects.
After your initial scan, you complete the stress test on a treadmill or stationary bicycle. If you can’t exercise, you’ll receive medication to make your heart work harder. After exercising, you undergo an additional scan.
A PET stress test can usually be performed in around 30 minutes.
The test usually takes three to four hours, but you exercise for less than 15 minutes.
After completing or stopping the test, healthcare providers monitor your symptoms, heart rate, blood pressure and ECG until it returns to a normal range. This takes about 15 minutes. Once your heart rate has recovered, you are free to go home.
If the results are normal, your heart is pumping as it should and there is adequate blood flow. What this means for your health depends on why you underwent stress testing:
Abnormal results may mean you have heart disease. For signs of mild heart disease, healthcare providers may recommend lifestyle changes (like smoking cessation or an exercise and weight loss program) and medications to treat your diabetes, blood pressure or cholesterol to lower the risk of it worsening.
If abnormalities occur during the early stages of the test or affect large segments of heart tissue, additional tests may be necessary. These include:
Abnormal results may also mean your heart is not strong enough for exercise or surgery. Additional therapies may be necessary to help you avoid a heart attack or heart failure.
A heart stress test is a method for evaluating heart function and blood flow. It involves exercising or taking medications that simulate the effects of exercise. There are many reasons you may need an exercise stress test, such as assessing coronary artery disease symptoms and monitoring treatments. It provides valuable information that protects your current and future heart health.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
