Ischemic cardiomyopathy is an issue with damaged heart muscle that can’t pump blood well. Most of the time, coronary artery disease causes this damage by not allowing enough oxygen-rich blood to get to your heart muscle. Treatments range from medicines to surgeries. Your outlook depends on how much the lack of oxygen injured your heart muscle.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
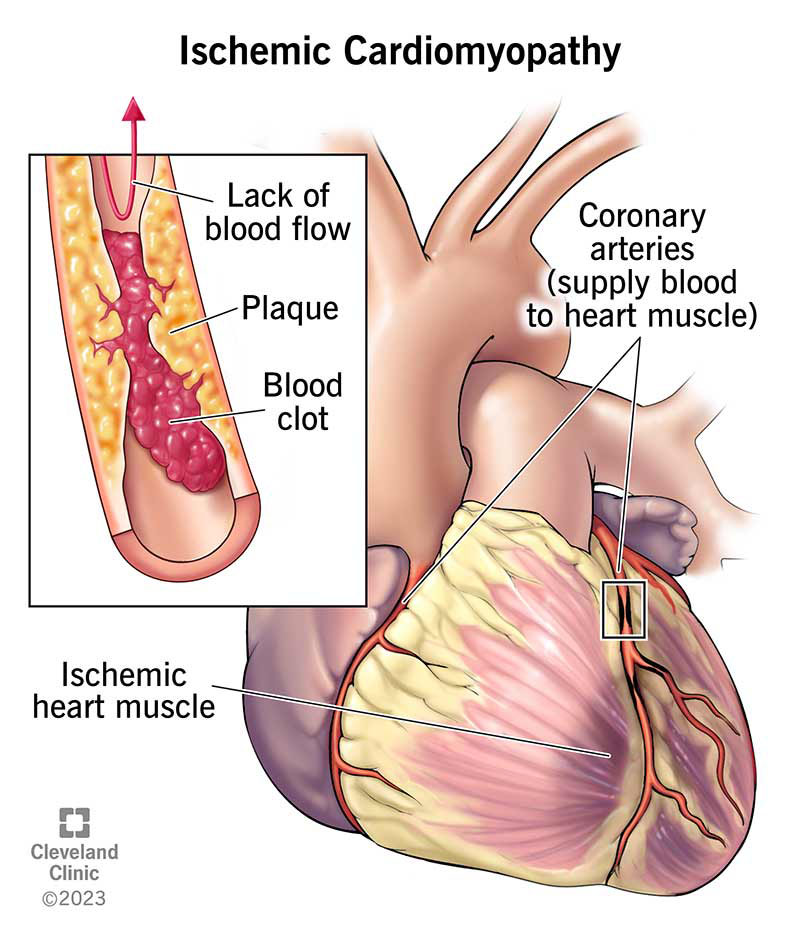
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17145-ischemic-cardiomyopathy-illustration)
Ischemic cardiomyopathy describes heart muscle that can’t pump well because of damage from a lack of blood supply to the muscle. Coronary artery disease and heart attacks cause this lack of blood supply (ischemia).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This lack of blood weakens and enlarges the left ventricle in people with ischemic cardiomyopathy. Because your left ventricle is your heart’s main pumping chamber, a weak left ventricle decreases your heart’s ability to pump blood.
Ischemic cardiomyopathy is the most common type of dilated cardiomyopathy and the world’s top cause of systolic heart failure. It causes 60% of cases.
Ischemic cardiomyopathy symptoms may include:
Some people may not have symptoms of ischemic cardiomyopathy.
Causes of ischemic cardiomyopathy are conditions that damage your heart muscle due to low blood flow, such as:
Major risk factors of heart disease can put you at an increased risk for cardiovascular (heart and blood vessel) disease and ischemic cardiomyopathy. These risk factors include:
Advertisement
Complications of ischemic cardiomyopathy include:
A healthcare provider will diagnose ischemic cardiomyopathy based on:
Specific tests to diagnose ischemic cardiomyopathy may include:
Occasionally, a provider may perform a myocardial biopsy to determine the cause of cardiomyopathy.
For ischemic cardiomyopathy treatment, healthcare providers focus on:
Treatments to decrease symptoms and improve quality of life may include:
Medications you take may include:
Medications can help:
Your provider will discuss what medications are best for you.
You can make changes in your daily routine that’ll improve your health. Changes include:
Some people need a device that can help their hearts work better. Types of devices include:
You may receive both devices combined in a single unit. This is a CRT-D.
Interventional procedures and surgeries include:
Side effects and complications vary by treatment:
Advertisement
Medications
Implantable devices
Procedures and surgeries
It can take a few weeks for a medication to reach its full effectiveness. Recovery times for other treatments can range from a day or so to several weeks or even months.
Depending on your situation, your heart muscle damage could be mild or severe.
Medications help your heart work better and ease your symptoms. But if these aren’t enough, your provider will recommend procedures or devices.
You may be able to reverse ischemic cardiomyopathy if you only have a lack of blood flow for a short time. But when your heart muscle doesn’t get enough blood and oxygen for a longer time, you can’t reverse the damage. This can happen when you have a heart attack.
The extent of damage to your heart muscle is a big factor in your prognosis. However, treatment can improve your situation. A provider will consider several things when talking about your outlook, such as:
Advertisement
You can prevent ischemic cardiomyopathy by preventing coronary artery disease. This is the most common cause of ischemic cardiomyopathy.
You can lower your risk of coronary artery disease and the cardiomyopathy it can cause by:
You have the power to make changes in your everyday life that improve your health. You can:
You’ll need to see your healthcare provider a few times a year so they can monitor your condition. Regular appointments help them see:
Advertisement
Between visits, contact your provider if:
Seek emergency care if you have:
Questions to ask your healthcare provider may include:
A diagnosis of ischemic cardiomyopathy can make you uneasy. But your healthcare provider can help you deal with it by suggesting the best treatment for you. And there are always things you can do to help yourself. Start by keeping your appointments and taking the medicines your provider prescribes for you. Ask your provider about anything you don’t understand about your condition.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you need treatment for coronary artery disease, you want expert care. At Cleveland Clinic, we’ll create a treatment plan that’s personalized to you.
