Pulmonary hypertension is high blood pressure in your lung arteries. It can result from heart disease, lung disease and many other health conditions. It can also happen for unknown reasons. You may have shortness of breath, dizziness and fatigue that get worse over time. Early diagnosis and treatment can help you manage symptoms and live longer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
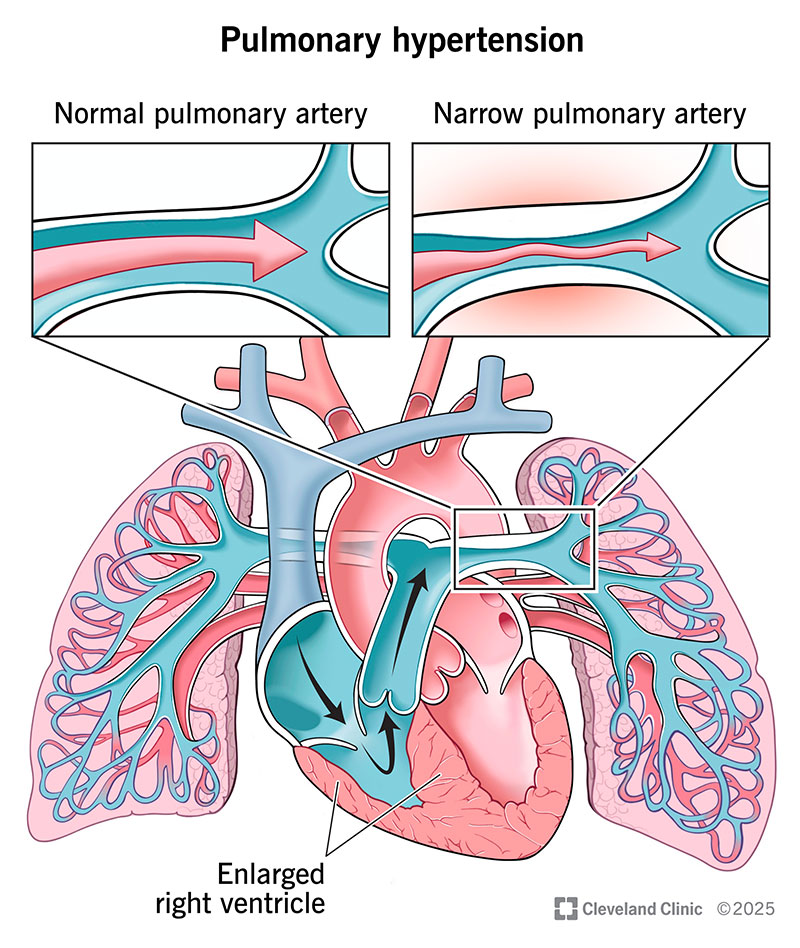
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/6530-pulmonary-hypertension-illustration)
Pulmonary hypertension (PH) means you have high blood pressure in your pulmonary arteries, which carry blood from your heart to your lungs. It has many possible causes, but it’s usually a complication of heart disease or lung disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Over time, the raised pressure damages your pulmonary arteries and narrows the space where blood can flow. This means your right ventricle (lower right heart chamber) must work harder to pump blood through those arteries so it can reach your lungs. This extra work makes your right ventricle get bigger than it should be (right ventricular hypertrophy), which may lead to right-sided heart failure. Without treatment, PH can be fatal.
The World Health Organization (WHO) divides pulmonary hypertension into five groups based on its cause:
Groups 2 and 3 are the most common. Group 1 (PAH) is rare, but people often confuse it with PH overall. That’s why you might hear that pulmonary hypertension is rare. It’s not. Experts estimate that PH affects about 1 in 100 people around the world. It’s most common among people over age 65. But it can affect anyone, including newborns, children and younger adults.
Advertisement
PH symptoms typically start off mild and get worse over time. No matter which type of PH you have, you might experience:
There are four main stages or “functional classes.” They’re based on your symptoms and ability to carry out your daily tasks. As PH gets worse, the symptoms become more obvious and disruptive.
There are five main types of PH — and each type has its own unique set of causes. Overall, heart and lung diseases are the most common ones. But you can also develop PH from other medical conditions or certain drugs or toxins. The exact cause matters because it determines your treatment plan. So, your healthcare provider will want to find out what it is.
Here are some lists of possible causes by PH type.
Group 1 (PAH):
Group 2 (left-sided heart disease):
Group 3 (lung diseases or hypoxia):
Group 4 (blockages in your lungs):
Group 5 (conditions that cause PH in complex or unclear ways):
Pulmonary hypertension can cause serious problems in your body, including:
Advertisement
Untreated PH is life-threatening. It’s important to get a diagnosis and start treatment as early as possible.
Healthcare providers diagnose pulmonary hypertension by doing a physical exam and running some tests. During the exam, your provider will check for signs of PH and other heart or lung issues by:
PH is difficult to diagnose. It shares signs with many other conditions. So, after your exam, your provider may do tests to learn more. You may need to see a lung or heart doctor for other tests.
Tests you may need to diagnose PH and its cause include:
Advertisement
Most cases of pulmonary hypertension can’t be cured. But treatment can help ease your symptoms, improve your quality of life and slow disease progression. You may need medications, procedures or surgeries to treat PH directly or target its cause. The exact treatments you’ll receive vary by PH type:
A lung transplant is a last resort for some people with pulmonary hypertension.
Pulmonary vasodilators are often a first-line treatment for people with PAH (group 1) and CTEPH (group 4). But they’re currently not FDA-approved for other groups. Researchers continue to look into medications that can help more people with PH.
Advertisement
Call your provider if you have:
Call 911 or your local emergency number if you experience:
Pulmonary hypertension is a progressive disease. That means it gets worse over time. It does this more quickly in some people than in others. Treatment can improve your chances of surviving for many years. Without treatment, PH leads to right-sided heart failure and is ultimately fatal.
Because PH can happen for so many reasons, the outlook is different from person to person. In general, your outlook depends on the type of PH you have, how early it’s diagnosed and other health conditions you have. Talk with your provider to learn more about what you can expect and how to manage your condition.
There’s a lot you can do to manage PH, take care of yourself and lower your risk of complications. Talk with your provider about:
This means the pressure in your pulmonary veins is too high. Despite its name, pulmonary venous hypertension isn’t a “type” of pulmonary hypertension (PH). Instead, it’s a common cause of PH — specifically, group 2 PH due to left-sided heart disease.
Your pulmonary veins carry blood from your lungs to the left side of your heart. But if there are problems on the left side of your heart, like heart failure or valve disease, blood can’t move through as easily. This causes blood to back up in your pulmonary veins as it waits its turn to enter your heart.
Over time, this can slow down the whole system of blood moving between your heart and lungs. Eventually, blood leaving your heart through your pulmonary arteries has to push harder to get through. This leads to raised pressure in those arteries and a PH diagnosis.
Learning you have pulmonary hypertension may make you feel scared, uncertain or overwhelmed. There’s a lot to learn. And starting new treatments or making changes in your daily life isn’t always easy. But your healthcare provider is there to guide and support you. Accept offers of help from family or friends to lighten your load. It’s OK to ask for help, too.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your child is diagnosed with pulmonary hypertension, you may have a lot of concerns and questions. Cleveland Clinic Children’s has the answers.
