Interstitial lung disease (ILD) is a group of conditions that cause inflammation and scarring in your lungs. The damage from it is usually irreversible. Symptoms include shortness of breath and a dry cough. ILD can be caused by medication, radiation therapy, connective tissue diseases or inhaling harmful substances.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
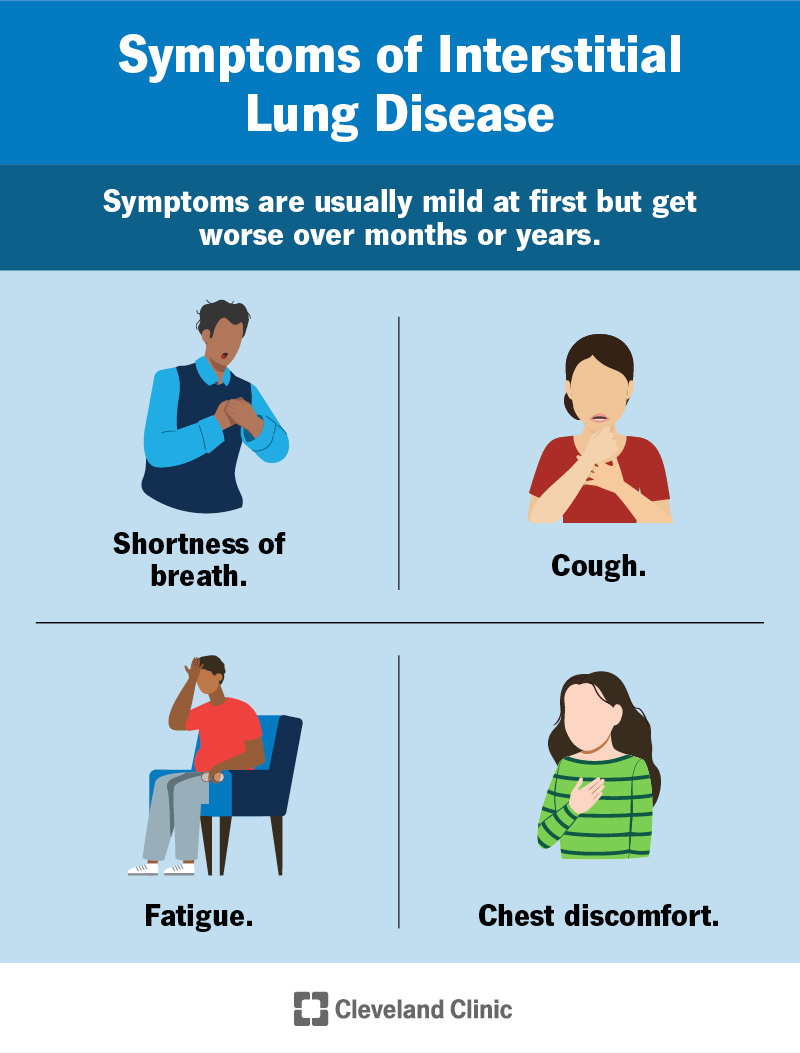
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17809-interstitial-lung-disease)
“Interstitial lung disease” (ILD) is a term for a group of conditions that cause inflammation and scarring in your lungs. ILD is the result of damage to the tissues between the small air sacs in your lungs (alveoli) and the blood vessels around them. This tissue is sometimes referred to as the intersitium or parenchyma.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The damage in ILD makes it hard for your lungs to get oxygen from the air to deliver to your tissues and to get carbon dioxide out of your body. This makes it hard to breathe. You might have a chronic cough or feel tired all the time. As damage gets worse, you can have life-threatening complications, like lung infections and respiratory failure.
Interstitial lung disease is different from conditions like COPD and asthma. These can have similar symptoms, but they affect your airways.
ILD is also called diffuse parenchymal lung disease (DPLD).
Examples include:
Common symptoms of interstitial lung disease include:
Symptoms are usually mild at first, but get worse over months or years. You may have additional symptoms depending on the underlying cause of ILD.
Advertisement
Healthcare providers usually describe the causes of interstitial lung disease as known or unknown. A known cause is when ILD happens because of another health condition you have or something you were exposed to, like certain medications, radiation or harmful substances.
Known causes of interstitial lung disease include:
An unknown cause is when you don’t have another health condition or exposures that caused ILD. This is called idiopathic interstitial pneumonia. There are many types. The most common is idiopathic pulmonary fibrosis.
You’re more likely to develop interstitial lung disease if you:
In severe cases of interstitial lung disease, you can have life-threatening complications, including:
Healthcare providers diagnose interstitial lung disease by:
They might ask you about:
Tests your provider may recommend include:
Advertisement
Treatment for ILD usually focuses on treating the underlying disease and improving your symptoms. This could include medications to reduce inflammation or slow down the disease. Your provider may also recommend treatments that can help improve your quality of life.
Treatments could include:
Advertisement
See your healthcare provider if you have symptoms that have gotten worse over time, an ongoing dry cough or shortness of breath that gets worse with exercise. The outlook for interstitial lung disease is best if treated as soon as possible.
Some forms of ILD aren’t reversible. Medications can help bring down inflammation depending on the type of ILD. And you might be able to slow down or prevent further damage.
How you and your healthcare provider treat ILD depends on the cause. For example:
The life expectancy for interstitial lung disease depends on the cause and severity. Some people with mild ILD live their lives as usual without treatment or with minimal treatment. Your outlook (prognosis) is better if the damage isn’t getting worse.
Advertisement
For people with the most severe and rapidly worsening forms of interstitial lung disease, life expectancy may be as low as three to five years after diagnosis.
Many causes of interstitial lung disease aren’t preventable. You can reduce your risk by managing underlying conditions and avoiding breathing in harmful substances.
There are dozens of types of interstitial lung disease (ILD). Some cases are mild, and some are very serious. You might find scary statistics online, but only your healthcare provider can tell you what to expect in your specific case. Having honest conversations with your provider can help set expectations. Together, you can make a plan to improve your symptoms and have the best quality of life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When breathing stops being natural and becomes difficult, it’s time to get help. Cleveland Clinic’s interstitial lung disease experts can help manage your symptoms.
