Langerhans cell histiocytosis is a rare disorder that occurs when a type of immune system cell called Langerhans cells build up in your child’s body. When these cells accumulate, it can cause tissue damage and tumors to form. The outlook for the disease depends on where the cells affect your child’s body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
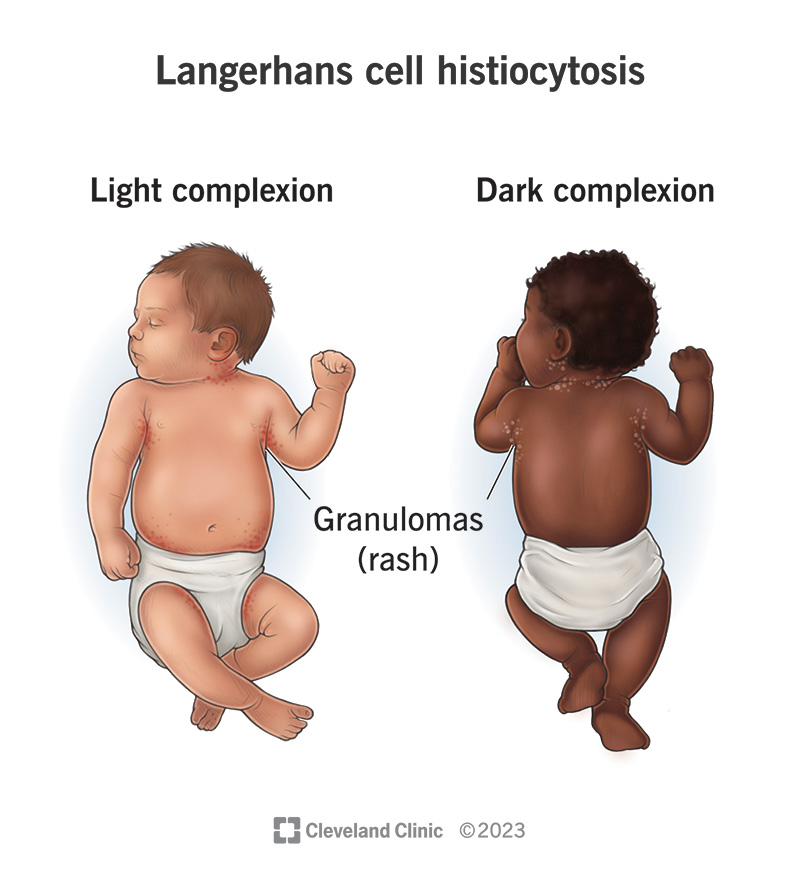
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/langerhans-cel-histiocytosis.jpg)
Langerhans cell histiocytosis (LCH) is a rare disorder that primarily affects babies and children. The disorder occurs when immune system cells called Langerhans cells build up in your child’s body. Langerhans cells are a type of white blood cell that helps your child’s immune system fight infection.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your child has Langerhans cells throughout their body, especially in their skin, lungs, lymph nodes, bone marrow, spleen and liver. When there’s a buildup of these cells, it can damage your child’s tissues and cause lesions to form in one or more places in their body.
The outlook (prognosis) of Langerhans cell histiocytosis is wide-ranging, but in general, is good. For many children with LCH, the disease goes away with appropriate treatment. In fact, it may go away on its own, especially if it only occurs in your child’s skin. But when LCH affects your child’s bone marrow, spleen or liver, the disease may require intensive therapy.
Many researchers consider Langerhans cell histiocytosis a type of neoplasm. But some have begun to consider it an inflammatory disease. Healthcare providers who treat cancer and blood disorders (oncologists) also treat Langerhans cell histiocytosis. Sometimes, oncologists use cancer therapies like chemotherapy to treat the condition.
Most cases of LCH affect newborns and children between the ages of 1 and 15 years old. Langerhans cell histiocytosis in adults is rare, but it can occur.
Langerhans cell histiocytosis occurs in 1 to 2 out of every 1 million newborns every year. It affects about 5 out of every 1 million children ages 15 and younger each year.
Advertisement
Langerhans cell histiocytosis varies greatly from person to person. It may involve only one part of your child’s body or many different sites. So, Langerhans cell histiocytosis symptoms will vary depending on which part of your child’s body is affected.
In about 80% of children with LCH, one or more lesions develop in their bones. This can cause swelling or a lump over a bone like your child’s skull, eye socket, ear bone, jaw bone, arms, legs, spine, hips or ribs. The swelling may or may not be painful. Additional symptoms affecting bones may include:
Langerhans cell histiocytosis skin symptoms typically include a rash. In infants, it may be a scalp rash that looks like cradle cap. In children and adults, a flaky rash may look like dandruff. Rashes may appear on other parts of your child’s body and be tender, painful or itching. Your child may have oozing blisters. Other areas of their body that may be affected include:
In addition, you may notice discoloration or hardening of your child’s nails or their nails may fall out.
Symptoms of Langerhans cell histiocytosis that may affect your child’s mouth include:
Symptoms of LCH that may affect your child’s liver and/or spleen include:
Signs of LCH that may affect your child’s bone marrow include:
Langerhans cell histiocytosis may affect your child’s endocrine system, including their pituitary gland and their thyroid gland. Symptoms that may affect these glands include:
Symptoms of LCH that may affect your child’s ears include:
Advertisement
Signs of Langerhans cell histiocytosis that may affect your child’s eyes include:
Signs of LCH that may affect your child’s lymph nodes include:
Symptoms of LCH that may affect your child’s brain and/or spinal cord (central nervous system) include:
Lung (pulmonary) Langerhans cell histiocytosis is more prevalent in adults. People who smoke are at a higher risk of developing pulmonary LCH. Signs of LCH in your lungs include:
Symptoms of Langerhans cell histiocytosis that may affect your child’s stomach, intestines and/or colon may include:
Because the cause of these symptoms could be another condition not related to Langerhans cell histiocytosis, it’s important to seek proper medical attention to receive an accurate diagnosis.
Advertisement
In about half of the people with LCH, a somatic mutation in the BRAF gene causes the condition. A somatic mutation is a change that occurs in certain cells after conception. (You don’t inherit these mutations — they happen randomly to a developing fetus.)
The BRAF gene is responsible for making a protein that controls cell growth and development. Normally, this protein can be switched on and off in response to chemical signals. A mutation in this gene causes the protein to be stuck in the “on” position, which causes too many LCH cells to grow and divide. This can cause tissue damage and the formation of tumors.
Scientists have discovered mutations in other genes that can lead to the disease as well. These include the MAP2K1, RAS and ARAF genes. Some researchers believe other factors, like environmental toxins and viral infections, may also lead to the development of the disorder.
Certain factors put your child at a higher risk of developing Langerhans cell histiocytosis. These include:
Advertisement
Almost 50% of children with Langerhans cell histiocytosis will experience complications due to the condition, including:
Your child's healthcare provider will ask about your child’s medical history and perform a physical exam. They’ll request several tests, depending on where your child has symptoms. Based on their findings, your child’s provider may refer you to a pediatric hematologist/oncologist, who’ll coordinate the care and treatment of your child.
Langerhans cell histiocytosis can affect many different parts of your child’s body. Therefore, your child may need several tests to diagnose the condition.
Treatment for Langerhans cell histiocytosis depends on where LCH cells are located in your child’s body and whether the condition is considered low-risk or high-risk.
Low-risk organs include:
High-risk organs include:
Healthcare providers classify LCH as single-system disease or multi-system disease. They classify the disease based on how many of your child’s body systems are affected:
In certain cases, LCH may improve on its own without treatment. This typically occurs in single-system LCH cases involving the skin or bone. In these cases, treatment involves observation to ensure the disease doesn’t return or spread.
Treatment options for LCH may include:
The prognosis for LCH depends on various factors, including:
Typically, providers consider children with single-system LCH and multi-system LCH that doesn’t involve the liver, spleen or bone marrow low risk. With treatment, the overall survival rate for children in this category is 100%. However, disease recurrence and/or other long-term complications are common.
Providers consider children with multi-system LCH that involves the liver, spleen or bone marrow high risk.
You can’t prevent Langerhans cell histiocytosis because a genetic mutation causes it. Some risk factors for LCH are things you can’t control like your biological family history and ethnicity. But there are some factors you can manage, like:
Even after your child completes treatment, their healthcare provider will want to see them regularly. They’ll want to monitor your child for many years because the disease has a high risk of coming back (recurring). At their follow-up appointments, your child will repeat many of the same tests they had when they received their diagnosis. These may include ultrasounds, MRIs, CT scans and PET scans. Your child’s provider will let you know how often you need to come back for follow-up.
You may have many questions about your child’s diagnosis. It may help to write them down to take with you to your child’s next appointment. A few questions you may want to ask include:
Langerhans cell histiocytosis (LCH) is a very rare condition that affects mostly children. If your child is one of those children, you may be overwhelmed with emotions. You may be worried for your child. You may be scared on the inside but trying to hold it together on the outside. All of your emotions are valid, but it may help to know you don’t have to do this alone. Your child’s care team knows what you’re going through. They’ll be with you to help you understand and cope with your child’s condition every step of the way.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Finding out you may have a rare blood condition like Langerhans cell histiocytosis can be a shock. Cleveland Clinic has the care and support you need.
