Hemostasis is your body’s way of stopping bleeding and making a repair after an injury. Seconds after an injury, your body starts the process of forming a plug or clot. Making a clot conserves blood and prevents infections. But in rare cases, the process doesn’t work as it should. This can cause problems with too much or too little clotting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
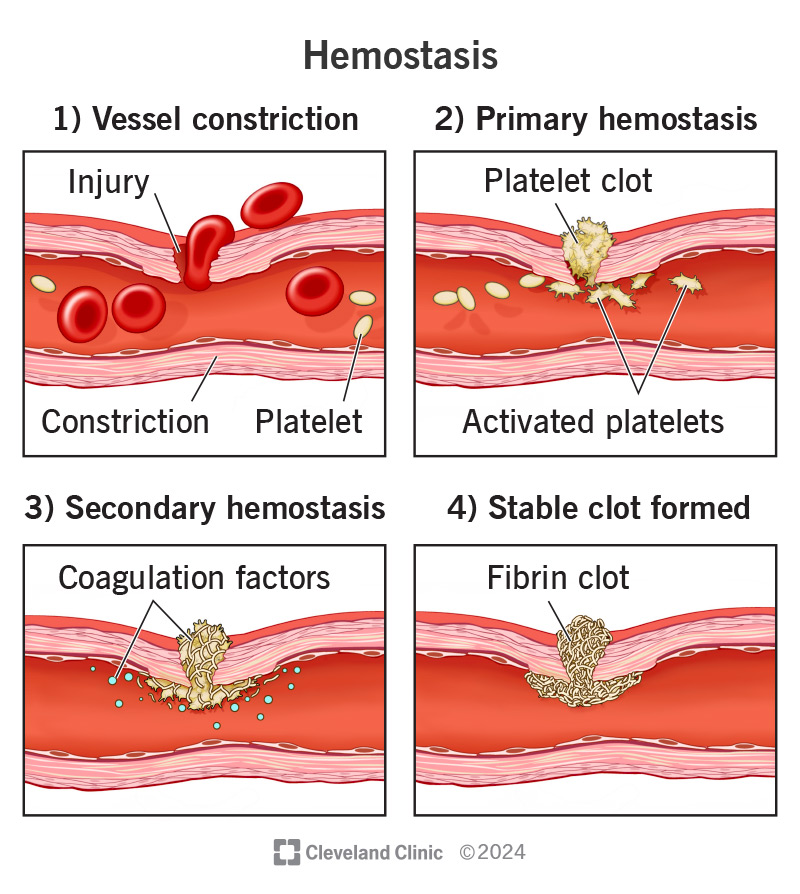
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/hemostasis)
Hemostasis (hee-muh-stay-sis) is your body’s normal reaction to an injury that causes bleeding. This reaction stops bleeding and allows your body to start repairs on the injury. You need this ability to stay alive, especially with significant injuries.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When all goes well, hemostasis is a good thing. But in uncommon cases, the processes that control hemostasis can malfunction. This can cause potentially serious — or even dangerous — problems with bleeding or clotting.
Hemostasis combines the terms “hemo” (meaning “blood”) and “stasis” (meaning “standing still”). In this context, it’s the term for how your body stops bleeding. The process starts just seconds after an injury. It’s normal for a wound to bleed for two to seven minutes.
The hemostasis process isn’t a single one, but a collection of several processes.
The steps of hemostasis include:
Advertisement
An injury triggers hemostasis. Your body naturally monitors itself for injuries. Any break in your skin is a risk for germs to enter your body. Clots help reduce that risk by sealing the injury. When your body detects an injury, it reacts quickly to take control of the situation. Without normal hemostasis, even minor injuries could cause dangerous blood loss. An example of this is hemophilia, a condition where hemostasis doesn’t work properly and blood can’t clot effectively.
Hemostasis refers to normal blood clotting in response to an injury. But your body can clot too little (hypocoagulability, in which you bleed or bruise too much in response to an injury). Or you can clot too much (hypercoagulability, in which you clot even without injury). Hypercoagulability can cause many blood clots to form spontaneously and block normal blood flow. When blood clots form inside your blood vessels, healthcare providers call it a thrombosis. If thrombosis happens repeatedly, you may have a condition called thrombophilia.
Hypercoagulability is when your blood clots too much or too easily. This is dangerous because those clots can get stuck in different places in your body and cause severe, life-threatening problems. Examples of these problems include:
Many types of cancer can cause hypercoagulability, as can some rare genetic conditions. That means you either inherit them from your parents or they happen because of a random variation in your DNA. People with these conditions have thrombophilia. A few examples of conditions like this include:
Inherited disorders that can cause thrombophilia aren’t as common as “acquired” conditions, which you usually develop later in life. Examples of acquired conditions include:
Most medications that treat thrombophilia make it harder for your blood to clot in some way. Examples of these include:
When your blood doesn’t clot well, any injury becomes a much more dangerous event. Without proper clotting, even minor injuries can cause you to lose a lot of blood. It also means you’re at a greater risk for injuries to organs and blood vessels inside your body, which can then cause internal bleeding.
Advertisement
Certain types of cancer, like leukemia, can cause you to bleed too easily. That’s because they often involve a lack of platelets in your body or anti-clotting activity. Conditions that keep your blood from clotting are often genetic, too. Some examples of genetic conditions include:
Treating conditions that keep your blood from clotting usually involves medications that slow down or block your body’s anti-clotting processes, boost your body’s ability to make platelets or add more of certain clotting factors to your blood. You can also receive transfusions of platelets to add more if your body needs them.
A healthcare provider — like a hematologist — can diagnose hemostasis problems based on your symptoms and blood tests that analyze the clotting-related components in your blood.
Blood tests may include:
Hypercoagulability can happen with a variety of different symptoms depending on where and when an abnormal clot develops. Examples of this include:
Advertisement
Hypocoagulability will cause you to bleed more easily. Most often, this causes the following symptoms:
Advertisement
We all bleed. Hemostasis is a natural part of your daily life — it’s what stops the bleeding so we can heal. It helps your body protect itself from infection and recover from injuries of all sizes. Understanding how it works can help you better care for yourself. It also means you can recognize potential problems with your body’s natural recovery abilities and get help sooner rather than later.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Blood clotting disorders can be genetic (inherited) or acquired. Cleveland Clinic’s experts diagnose and treat these disorders to lower your risk of complications.
