Thrombophilia is a condition that makes your blood more likely to form clots. Blood clots help you heal, but cause issues when they happen too easily or last too long. They can keep blood from moving where it needs to go. Blood thinners can prevent or treat blood clots, whether you have an inherited or acquired type of thrombophilia.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
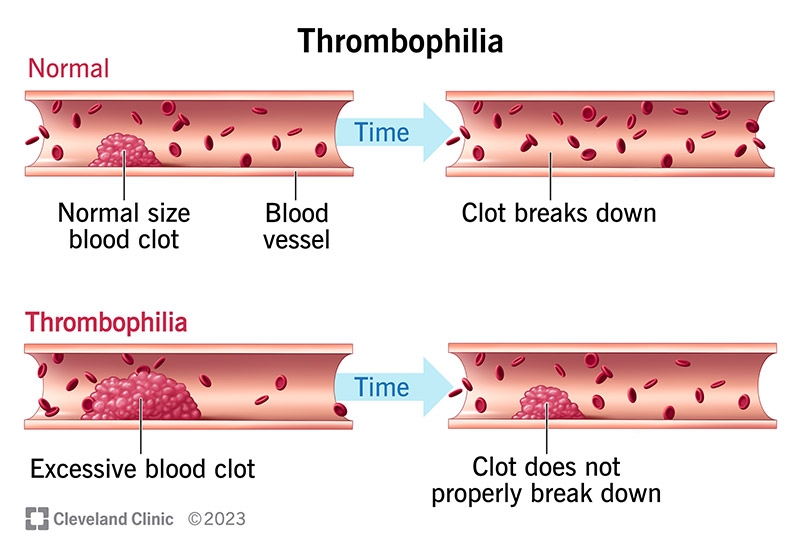
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21797-thrombophilia-illustration)
Thrombophilia is a blood disorder that makes the blood in your veins and arteries more likely to clot. Healthcare providers call this a “hypercoagulable” condition because your blood coagulates or clots more easily. Thrombophilia can be an inherited (genetic) or acquired tendency to form blood clots in arteries and veins.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Normally, your body makes a blood clot when you cut your finger with a knife, for example. The blood clot stops the bleeding. Later, your body breaks the clot apart when it doesn’t need it anymore. When you have thrombophilia, your body makes too many blood clots or doesn’t break down the old ones.
Blood clots can cause clogs or blockages in your veins or arteries. This can hurt your major organs or cause a stroke or heart attack because your blood vessels carry the oxygen your cells need. A clog in your blood vessel keeps blood from getting to your cells.
There are two types of thrombophilia: the kind you’re born with (genetic) and the kind you get (acquired) in other ways.
Advertisement
Types of genetic thrombophilia include:
You may not feel any thrombophilia symptoms unless you get a blood clot. Blood clot symptoms differ in various parts of your body:
Brain
Heart
Lungs
Belly
Leg or arm
In addition to a genetic problem with a protein your body uses for clotting, causes of thrombophilia include other medical issues, like:
Thrombophilia risk factors include:
Advertisement
Blood clots can travel all over your body, limiting or blocking blood flow to your organs. This can cause serious problems in your:
Your provider can make a thrombophilia diagnosis with:
You should get a test for thrombophilia if you get a blood clot and:
Some conditions can give you a false positive test result, so make sure your provider knows your full medical history. Conditions that can affect test results include:
Advertisement
Your provider may order thrombophilia testing that includes:
Although you can’t cure the kind of thrombophilia that you inherit, you can treat it.
Thrombophilia treatment for acquired or inherited types of the condition may include compression stockings for your legs or medicine to prevent or break up a blood clot. Some people may need surgery to remove a blood clot.
Providers order medications, such as:
Side effects of blood thinners may include:
It’s important to know that blood thinners don’t dissolve blood clots. They stabilize the blood clots so they don’t move or get bigger, and allow your body’s natural resources to absorb the clot over time.
But thrombolytics you get through an IV can dissolve clots quickly.
Advertisement
Although your provider can’t cure genetic thrombophilia, they can order medicine like blood thinners for you to take for life. This medicine will help you manage your thrombophilia.
Nearly 90% of people who have thrombophilia never get a blood clot, but some people get one or more serious clots.
If you inherited thrombophilia, you’ll have it for life. Other kinds of thrombophilia can improve when you treat the condition that caused it.
You can’t prevent thrombophilia that you got from your parents, but you may be able to prevent some acquired thrombophilias.
If you’re at a high risk of blood clots, your provider may give you:
You can lower your risk of acquired thrombophilia on your own by:
If you have thrombophilia, you may need to take medicine for life. You also need to be careful in situations where you could get a cut, like during meal preparation.
You may need to take blood thinners if your risk of forming more blood clots is high. With some of these medicines, you’ll need to have frequent checkups.
You may also want to find safer ways to cut food, brush your teeth or shave to prevent bleeding.
Contact your provider if you think you’re having any of the signs and symptoms of a blood clot, including:
Contact your provider right away if you have issues with the blood thinner you’re taking, like nosebleeds or blood in your urine (pee) or poop.
Get emergency medical treatment if you think you’re having a stroke, heart attack or pulmonary embolism (blood clot in your lungs).
If you have thrombophilia, your blood clots too easily. If you have hemophilia, your blood doesn’t clot easily enough.
Being pregnant increases your risk of clots and a thromboembolism, even if you don’t have thrombophilia. Although there isn’t a strong link between having genetic thrombophilia and having preeclampsia or stillbirth, your provider may want to give you an anticoagulant to keep you from having a venous thromboembolism. There are specific anticoagulants, like heparin or enoxaparin, that are safe for the fetus.
Blood clots are scary. While you’ll need to take some precautions, worrying about blood clots doesn’t have to take over your life. Many people with this disorder never get a blood clot. You can manage thrombophilia with medicine, but be sure to keep all of your follow-up appointments with your provider. If you have thrombophilia in your family, check with your provider to see if they want to screen you for it.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Blood clotting disorders can be genetic (inherited) or acquired. Cleveland Clinic’s experts diagnose and treat these disorders to lower your risk of complications.
