Thrombosis is a serious condition where one or more blood clots form in your blood vessels or heart. When this happens, the clot can block blood flow where it formed, or it can break loose and travel elsewhere in your body. If a moving clot gets stuck in a critical area, it can cause life-threatening conditions like stroke and heart attack.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
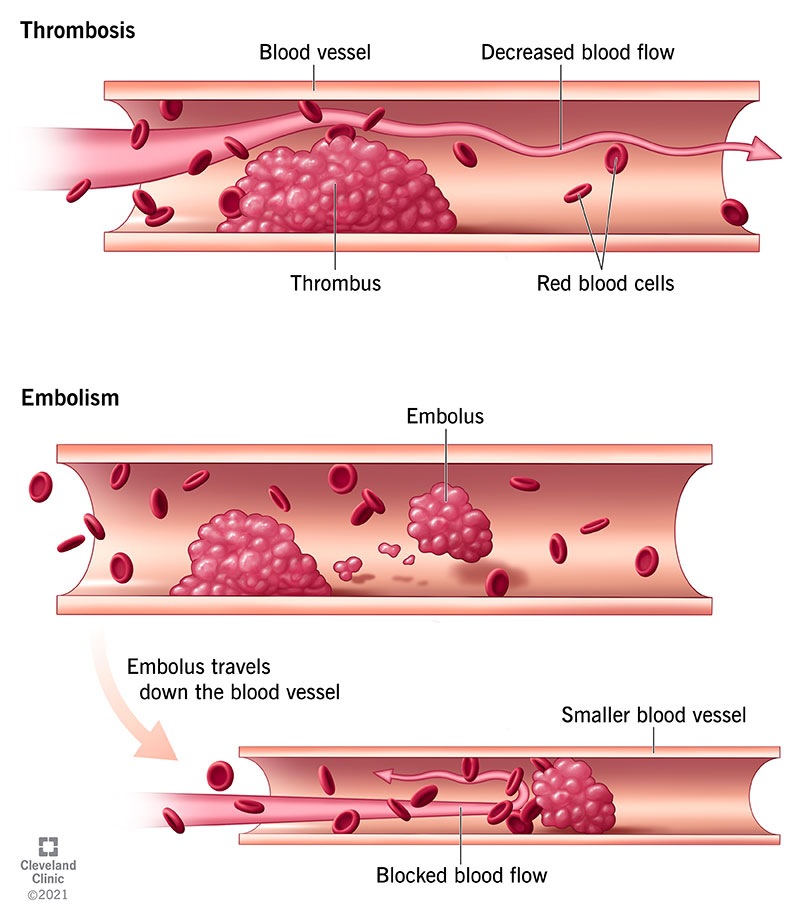
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22242-thrombosis-illustration)
Thrombosis is the formation of a blood clot (thrombus) inside one of your blood vessels or a chamber of your heart. Clots can block blood flow in your blood vessels or break free and travel elsewhere in your body. If a clot gets stuck in a critical location like your lungs or brain, it can disrupt blood flow to that organ and result in a life-threatening emergency. Symptoms vary based on the clot’s location and can include chest pain, trouble breathing and skin changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some people face a higher risk of thrombosis due to medical conditions or other factors. Learning your risk can help you prevent thrombosis, and learning the symptoms can help you recognize problems if they occur.
Thrombosis is a serious condition, and it can become more dangerous as time passes. It can quickly turn into a medical emergency. The sooner you seek care for thrombosis, the better your chances of a good outcome.
If you or someone with you has symptoms of thrombosis, seek emergency medical care immediately.
Thrombosis can lead to many different complications depending on where the blood clot forms or travels to:
The two main types of thrombosis are:
Advertisement
Thrombosis is dangerous in either location (artery or vein) because it can:
Thrombosis is extremely common and is the underlying cause of 1 in 4 deaths worldwide. That’s because thrombosis can lead to dangerous conditions like a heart attack, stroke or pulmonary embolism.
Thrombosis is more common among people with certain medical conditions, including:
Thrombosis symptoms depend on the size of the clot, its location (where it forms or gets stuck) and the complications it causes. Blockages are more likely to occur in areas with very small blood vessels, especially your lungs, brain and farther down in your legs and arms. Listed below are common symptoms for each location:
Lungs (pulmonary embolism)
Brain or neck [transient ischemic attack (TIA) or stroke]
Heart (heart attack)
Belly (mesenteric ischemia)
Artery in arm or leg
Vein in arm or leg
Advertisement
Thrombosis happens when something damages the inner lining of your blood vessel (endothelium) or slows blood flow. In either case, cells in your blood start to stick together when they shouldn’t.
Normally, many cells in your blood coexist in harmony and come together when needed for a certain job. For example, if you have a wound, platelets and proteins join together at the site of injury to serve as a plug. This multistage process (hemostasis) forms a necessary clot that stops you from losing too much blood. The clot dissolves when your wound heals. It’s like an emergency meeting at work when everyone huddles at one desk. When the problem’s solved, everyone leaves and goes their separate ways.
But various medical conditions, medications and other factors can cause components of your blood to cluster together when they don’t need to or fail to dissolve when they should. As a result, a blood clot (thrombus) may form from clumps of blood clotting components and potentially get bigger. It may also break away and travel through your bloodstream until it gets stuck in a smaller blood vessel (embolus).
Both of these situations can lead to dangerous — or even life-threatening — complications. That’s why it’s important to learn what may put you at risk.
Advertisement
Anything that interferes with your blood’s ability to flow freely or clot normally can raise your risk for thrombosis. This includes many conditions, medications and lifestyle factors.
Specific risk factors include:
Healthcare providers diagnose thrombosis based on:
During a physical exam, a provider will:
Advertisement
Imaging tests let your provider see inside your body. Possible tests you may need include:
Blood tests can show if your blood clots too easily and help your provider figure out why. These tests usually look for the following:
Thrombosis treatments include medications, minimally invasive procedures and surgeries. Your provider will tailor treatment to your needs.
Possible treatments include:
You may also need additional treatments for complications of thrombosis. Your provider can explain what you might need and why it’s necessary.
Most people who receive treatment feel better as they’re treated, especially as blood returns to previously blocked areas. That can happen in minutes or hours, depending on the location and size of the clot and the specific treatments.
In cases where you had severe effects from a clot, like a heart attack or stroke, it may be a few days before you start feeling better. That’s especially true if you need surgery or more intensive procedures and care.
Your healthcare provider is the person who best understands your case. They can tell you more about what to expect in your specific circumstances.
Early diagnosis and treatment can restore your blood flow and lower your chance of complications. If a complication (like a heart attack or stroke) leads to your diagnosis, your provider will treat that condition and do whatever possible to restore function to affected organs and tissues.
It depends on the underlying cause, the treatments and how quickly you seek medical attention. Thrombosis can be short-lived with prompt treatment. However, the conditions that cause it may be chronic or lifelong. For example, blood clotting disorders that you’re born with may put you at risk for thrombosis throughout life. Your provider can help you manage underlying conditions to lower your risk.
Your outlook or prognosis depends on many factors, including:
A clot that stays in place is a problem, but it’s usually less dangerous than a clot traveling in your bloodstream. The outlook for thrombosis can worsen when a free-floating clot ends up in a critical organ like your heart, brain or lungs.
Your provider can tell you more about your prognosis based on your individual situation.
When you know you’re at risk for clots, prevention is much easier. The best way to know about your risk is to get an annual physical (wellness visit or checkup). Your provider can detect many conditions that raise your risk for thrombosis long before clots form and offer guidance on prevention.
Your provider may recommend:
If you’ve had thrombosis in the past or are at risk, it’s crucial to:
Call 911 or your local emergency number if you have symptoms of thrombosis. Don’t delay. Thrombosis can very easily become a dangerous, life-threatening condition. The more minutes that pass, the greater the risk of complications.
Thrombosis is a condition that can quickly become a life-threatening emergency. The most important thing you can do is try to prevent thrombosis. While you can’t always prevent it, knowing the symptoms can help you recognize when to seek immediate medical care.
If you’ve had thrombosis in the past, you may worry about what the future will bring. Share your questions and concerns with your provider. They’re your best source of information about what you can expect in your specific situation.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
