Aortic dissection is a tear in the inner layer of a weak area of your aorta. Blood going through the tear splits your aorta’s layers. Your aorta is the main artery that delivers oxygen-rich blood to your body. Aortic dissection is a life-threatening condition that requires immediate care. Treatment includes several types of surgery and medication.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
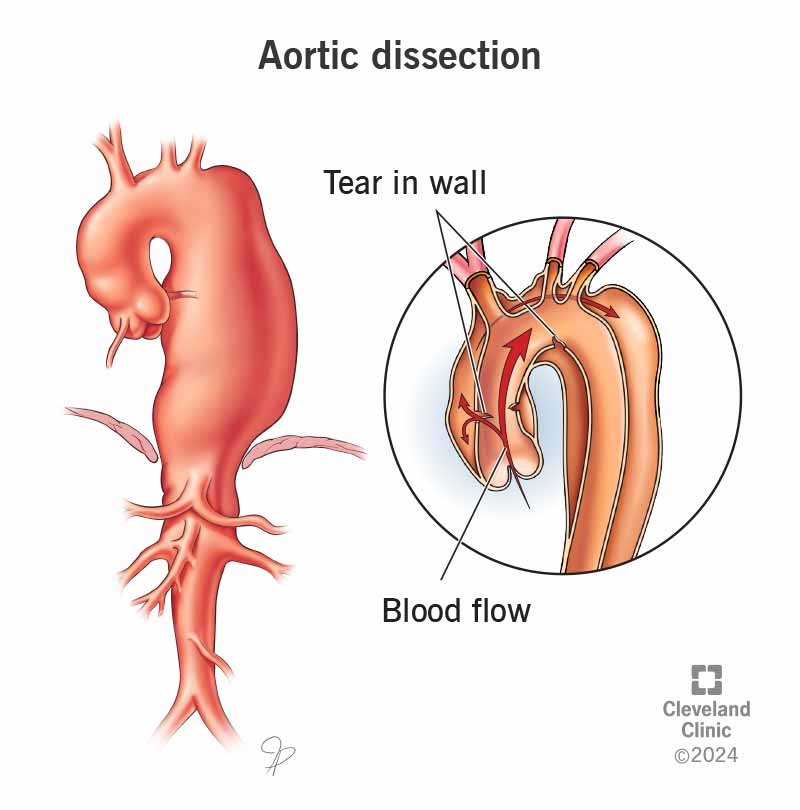
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/aortic-dissection-illustration)
An aortic dissection is a tear in your aorta. This is the main artery that carries oxygen-rich blood away from your heart to the rest of your body. It runs through your chest and abdomen and down to your legs. A rare condition, an aortic dissection begins abruptly when a tear happens in the inner layer of a weakened area of your aorta. Blood surges through the tear, causing the inner and middle layers (your aorta wall has three) to separate (dissect).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As diverted blood flows between the tissue layers, the normal blood flow to parts of your body may slow or stop, or your aorta may rupture completely.
Without quick diagnosis and care, an aortic dissection can cause sudden death. This is a life-threatening condition. Get emergency treatment right away. You may feel scared, but first responders will know what to do.
Each year, 5 to 30 people per 1 million have an aortic dissection.
There are two main aortic dissection types:
Advertisement
Healthcare providers also use the DeBakey classification system, which has three types. Type 1 starts in your ascending aorta and extends through your descending aorta. Type 2 starts in and is limited to the ascending aorta (both would be considered Stanford Type A). Type 3 starts in your descending aorta and extends downward (like Type B).
The most common feature of aortic dissection is its abrupt start. It can happen at any time, most commonly from a sudden rise in blood pressure with heavy exertion. But it can occur while doing anything, at rest or when you’re sleeping. There are no aortic dissection warning signs.
Common aortic dissection symptoms you may experience include:
If you have symptoms of aortic dissection, severe chest pain or symptoms of a stroke, call 911 or your local emergency services number, or seek emergency care.
Aortic dissection happens because there’s a slow breakdown of the cells in the walls of your aorta. The breakdown has likely been going on silently for many years before the weakened area of the aortic wall finally gives way. This results in a tear, which leads to the aortic dissection.
Healthcare providers believe that a basic weakness in the aortic wall (possibly inherited) causes most aortic dissections. In other cases, the stress from constant high blood pressure can weaken the aorta wall. This can lead to a tear and dissection.
Tears in the aorta typically occur in areas where the stress on the wall of the aorta is highest, like your ascending aorta. Aortic dissection in the ascending aorta is nearly two times more common than those that happen in the descending aorta.
Factors that can increase your risk of an aortic dissection include:
Advertisement
Powerlifting may increase how quickly aneurysms or dissection develop in people who are prone to them.
If you have high-risk factors (like aneurysms or a connective tissue disorder), look for an aortic center of excellence for your care. These centers have access to the latest innovations for treatment. They also offer the best in multidisciplinary care (including cardiologists, imaging specialists and geneticists). Multiple studies have demonstrated that centers that treat a lot of aortas provide the best outcomes for these complex cases.
Aortic dissection can lead to:
A provider may suspect an aortic dissection based on the symptoms you’re having. But they need to determine if you have aortic dissection or other health issues, like heart attack and stroke, which produce similar symptoms. With aortic dissection, it may be hard to find a pulse in your arms and legs. A provider may find that the blood pressure in one arm is higher than the other.
Providers need to diagnose aortic dissection quickly in case you need immediate surgery. When your team makes an aortic dissection diagnosis, a critical care transport team may transfer you to a center that manages these complex conditions.
Advertisement
A provider may order tests including:
Advertisement
Aortic dissection treatment depends on the location of the tear and dissection.
Surgical options include:
A provider may prescribe medications like beta-blockers to lower your heart rate and blood pressure. In some Type B aortic dissection cases, they may use medication alone to treat the dissection at first. A provider may delay surgery for months to years depending on the severity of the tear and extent of dissection.
Aortic dissection can be a life-threatening event. People who have acute aortic dissection (sudden onset, Type A) have a high death rate. About 40% of people with Type A aortic dissection die immediately from complete rupture and bleeding out from their aorta.
People who survive the acute phase usually have a chronic dissection remaining in the untreated portions of their aorta. This may require later treatment.
With modern advances in care, the prognosis (outlook) in the chronic phase is improving. But life expectancy after aortic dissection is shorter compared to the general population. Still, with early treatment and management by a trained aortic team, people can live normal lives for many, many years after an aortic dissection.
You can’t change many of the factors that increase the risk of developing aortic dissection. These include being born with certain heart conditions, connective tissue disorders, or genetic triggers associated with having a family history of aortic dissection.
But you can decrease some of your risks by:
If you get an aortic aneurysm diagnosis, seek out a healthcare provider (cardiologist or cardiac surgeon) who specializes in aortic disease. They’ll be able to assess your risks and use imaging to carefully monitor you for the need for elective repair of your aorta.
A provider will prescribe blood pressure medicine, usually beta-blockers, to manage your blood pressure and heart rate. You’ll need to take them for the rest of your life. You may need more than one blood pressure medication.
Avoiding tobacco products is important after an aortic dissection, too.
It’s OK to do aerobic activities like walking, biking and swimming. But you’ll need to avoid certain activities, like heavy weightlifting (more than half your body weight). They can increase your blood pressure and put added stress on your aorta.
When you survive aortic dissection — even if you don’t have surgery — you need to see a provider regularly (usually, every three to 12 months) for follow-up imaging with a CT or MRI. This allows providers to catch changes and act on them quickly.
Questions you may want to ask your provider include:
An aortic aneurysm is a bulge — like a bubble or a balloon — in a weakened area of the wall of your aorta or across an entire segment of your aorta. Aortic aneurysm can lead to aortic rupture and aortic dissection.
An aortic rupture is a complete tear through all three layers of the aorta — like a rip or a hole — in the wall of your aorta. Blood bursts through the hole into the area around it.
An aortic dissection is a tear in the inner aortic layer. It allows blood to enter and further separate the inner and middle layers of the wall of the aorta. It typically extends over a long length of your aorta in either direction and may extend into branch vessels that start in your aorta.
Having an aortic dissection is a scary and bewildering experience. Surviving it can bring a range of emotions. Your feelings are valid and there are others who understand what you’re going through. Be your own advocate and ask questions about anything that isn’t clear. Keep taking your medications and following all instructions from your healthcare provider. Be sure to keep all your follow-up appointments.
It’s important to go to an aortic center of excellence that has a lot of experience and has a multidisciplinary approach to care. Outcomes at these aortic centers are far superior to those with very few cases.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When you come to Cleveland Clinic for aortic disease treatment, you’ll get industry-leading care and support from our heart and vascular specialists.
