Ischemic strokes happen when a blood clot blocks a blood vessel in your brain. They are medical emergencies and can be fatal. Call emergency services right away if you think you or someone you’re with is experiencing stroke symptoms. The sooner you get treatment, the better your chances of survival.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
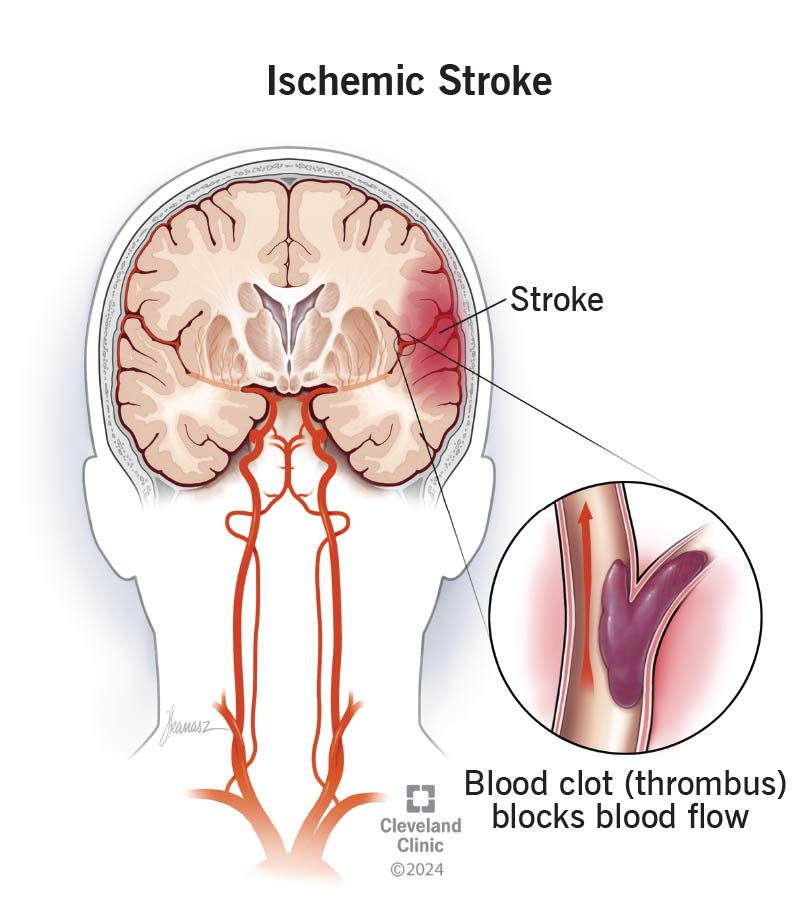
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/ischemic-stroke)
An ischemic stroke happens when something blocks blood flow from getting to your brain. It’s a life-threatening medical emergency.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ischemic strokes can cause permanent brain damage and death. If enough brain cells die, you can lose the abilities or body functions those cells control. They’re the most common type of stroke — around 80% of all strokes.
If you think you or someone you’re with is having a stroke, immediately call 911 (or your local emergency services number). The sooner someone is diagnosed and treated, the more likely they’ll survive a stroke. Every second counts.
The ischemic stroke symptoms you experience will depend on which area of your brain it affects. Some of the most common symptoms include:
Ischemic strokes can cause lots of different symptoms. To recognize the warning signs in yourself or a loved one, remember the acronym BE FAST:
Advertisement
Ischemic strokes happen when something causes ischemia in your brain. Ischemia (pronounced “iss-KEY-me-uh”) is the medical term for cells not getting enough blood and dying. Blood clots are the most common cause.
Many health conditions can cause blood clots, such as:
There are two types of ischemic strokes:
Transient ischemic attack
A transient ischemic attack (TIA) — sometimes called a “mini-stroke” — is like a stroke, but the effects are temporary. These are often warning signs that a person has a very high risk of having a true permanent stroke soon. A person who has a TIA needs emergency medical care as quickly as possible.
Anybody can experience an ischemic stroke, but some groups have a higher risk, including people who:
Having certain health conditions can increase your risk, including:
A healthcare provider will diagnose an ischemic stroke with a neurological exam and some tests. Providers in the emergency room may diagnose it if emergency services transport you to the ER.
Your provider will use some of the following tests to confirm that you’ve had an ischemic stroke:
The most important part of treating an ischemic stroke is restoring blood flow to your brain. Healthcare providers will do this as fast as possible to reduce your risk of permanent brain damage and death.
Advertisement
The two most common treatments include:
You may need other treatments, including:
Advertisement
Stroke rehab is an important part of treating an ischemic stroke. You’ll need stroke rehab to help you adjust to changes in your brain and body after a stroke. You may need to regain abilities you had before or adjust to new or different disabilities. You might need a combination of:
It’s hard for experts to estimate a survival rate that applies to everyone. Ischemic strokes can be fatal and can cause permanent disabilities. But there’s no one set recovery timeline or outlook that’s accurate for everyone.
Ischemic strokes usually have better outcomes than hemorrhagic strokes, but that doesn’t mean your recovery will be automatically easier, faster or better.
Everyone’s body responds differently to a stroke. What you can expect (the prognosis) after a stroke depends on a few factors, including:
Advertisement
Most people take a few months to recover after a stroke. The most recovery usually happens in the first three to six months after a stroke. But it’s possible that symptoms and after-effects can linger for a year or longer. A stroke can also cause permanent disabilities and other changes in how you can use your body.
Your provider will tell you what to expect. They’ll help you set recovery goals and expectations that fit your unique health and situation.
Maintaining your overall health is the best way to reduce your ischemic stroke risk. Try to:
Visit a healthcare provider for a checkup every year (or as often as they suggest). Many of the health conditions and issues that can cause ischemic strokes develop and build up over time, and may not cause symptoms you can notice. Lots of people with high blood pressure or high cholesterol never feel or sense anything wrong. Your provider can help you catch and manage any warning signs before they increase your risk of a stroke later on.
Recovering and rehabbing after a stroke is hard work. Once you and your provider finalize your treatment plan, follow it as closely as possible. In general, you should:
Your provider may suggest you add or remove some foods and drinks to your eating plan. They might suggest tweaks to your routine to help you manage health conditions you have and/or to lower your risk of future blood clots after an ischemic stroke.
Common foods you might need to avoid include:
Call 911 (or your local emergency services number) if you think you’re experiencing stroke symptoms again. Another stroke has an even higher risk of causing severe complications and being fatal. Don’t wait to call for help or go to the emergency room.
People who’ve had an ischemic stroke have an increased risk of other potentially serious complications, including:
Call emergency services or go to the ER if you think you’re experiencing any symptoms of these complications.
A stroke can be a scary, life-changing event. The best way to prevent an ischemic stroke is to catch the warning signs of a clot before they cause a stroke. See a healthcare provider at least every year, and ask them for help managing any conditions you have that increase your stroke risk.
If you’ve had a stroke, it can feel like your world is changed forever. But you’re still you. Recovery and rehab are hard work. Some days may be harder than others, but remember to stop and celebrate your successes and milestones.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
After a stroke, it’s essential to get treated right away. Cleveland Clinic’s stroke care specialists can help you manage recovery and improve your quality of life.
