Ear pain is one of the most common reasons we visit our healthcare providers every year. Earaches can be a symptom of infection or an underlying health condition. Most of the time, ear pain isn’t dangerous. Rarely, it’s a sign of a serious illness. Treatment depends on the cause but may include medication, home remedies or heat and cold therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
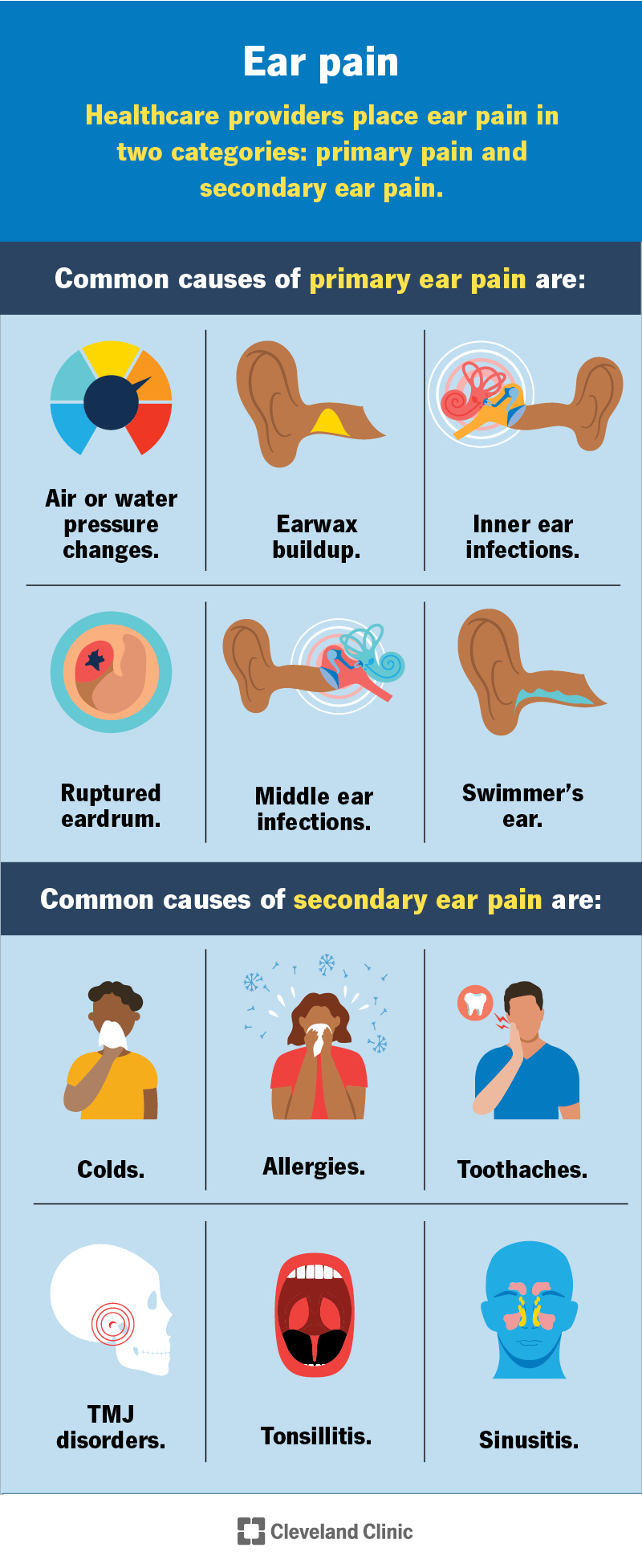
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/ear-pain)
Ear pain (an earache) is a symptom of many health conditions. It could point to an underlying issue. Or it might mean you have an ear infection.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Otalgia” (oh-TAL-gee-uh) is the medical name for ear pain. This pain might be dull, sharp, mild or severe. Some people have ear pain that comes and goes.
Most of the time, ear pain isn’t dangerous. But frequent earaches or pain that lasts longer than three days could point to something more serious.
Many things can make your ears hurt. Healthcare providers place ear pain in two categories:
Common causes of primary ear pain are:
Common causes of secondary ear pain are:
Ear pain isn’t always a sign of something serious. But if it lingers for more than three days, you should see your healthcare provider. If you have an infection, it can spread to nearby structures like your jaw or skull. Left untreated, ear infections can lead to serious complications like mastoiditis or meningitis.
Advertisement
Earache treatment depends on the cause. Over-the-counter (OTC) medications like acetaminophen (Tylenol®) or ibuprofen (Advil®) may be all you need for ear pain relief. But in some cases, your provider may prescribe medications in ear drops or pill form. These include:
Sometimes, rest and a little TLC can do wonders. You can try these home remedies to soothe ear pain:
Earaches happen for many reasons, and you can’t always avoid them. But doing the following may reduce your overall risk for ear pain:
Sometimes, earaches go away on their own. But if you still have ear pain after three days, you should call your healthcare provider. You should also tell them if you develop:
If your child has something stuck in their ear, schedule a visit with their pediatrician right away. This is especially true if you’ve tried to remove the object once with no success. Repeated removal attempts can increase the risk of ear injury. If you remove the object successfully, you should still call your healthcare provider if your child has symptoms like pain, ear drainage or muffled hearing.
When you have unbearable ear pain, it’s hard to think about anything else. Sometimes, over-the-counter pain relievers do the trick. But when ear pain lingers for days or comes back frequently, it’s time to tell your healthcare provider. In most cases, having an earache isn’t serious. But you shouldn’t ignore it. Prompt treatment can eliminate pain and infection and reduce your risk of associated complications.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have conditions affecting your ears, nose and throat, you want experts you can trust. Cleveland Clinic’s otolaryngology specialists can help.
