Tardive dyskinesia is a movement disorder that can develop if you take an antipsychotic medication and/or other types of medications. It’s typically not reversible, but treatment may help manage the symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Tardive dyskinesia (TD) is a neurological condition that causes movements you can’t control. It most often happens after long-term use of antipsychotic (neuroleptic) medications. But other medications can cause it as well.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Tardive” means delayed or late. “Dyskinesia” refers to involuntary movements. With this condition, symptoms usually don’t start right away. There’s often a delay between when you begin a medication and when the movements appear. Many people take the medication for years before developing tardive dyskinesia. But some people, especially older adults, may develop it after short-term use.
Researchers estimate that at least 20% of people who take first-generation (typical) antipsychotic medications develop tardive dyskinesia. The risk is lower with newer, second-generation (atypical) antipsychotics, but it can still happen.
It’s hard to know the exact risk for each medication because studies look at different groups of people and use different research methods.
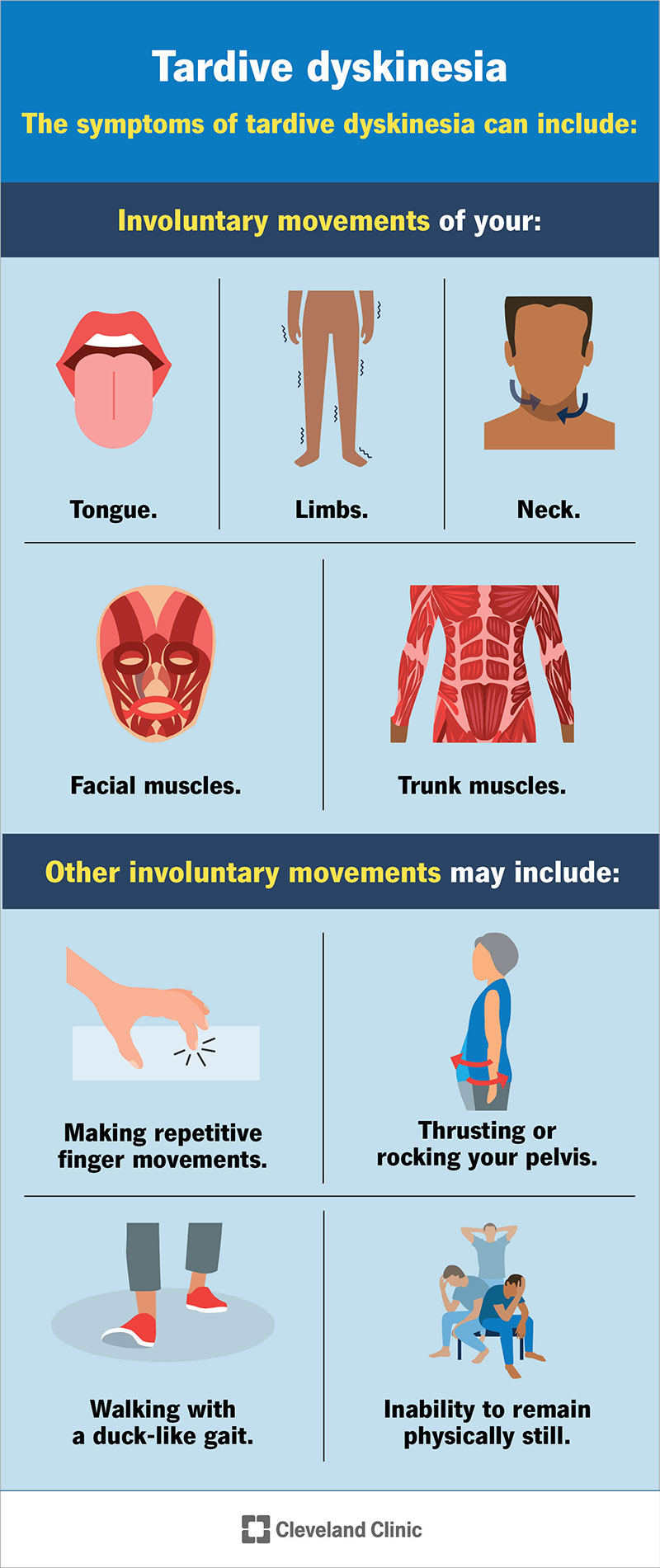
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/tardive-dyskinesia-infographic)
Tardive dyskinesia causes involuntary movements of your:
Facial involuntary movements may include:
Other involuntary movements may include:
Advertisement
These symptoms can be mild and barely noticeable or severe and disabling.
Your healthcare provider may use other terms to describe these movements, including:
Researchers don’t know the exact cause of tardive dyskinesia. But the leading theory involves dopamine, a brain chemical that helps control movement.
Some medications block dopamine receptors in your brain. Over time, this may make those receptors overly sensitive. This change can lead to the repetitive, uncontrolled movements seen in tardive dyskinesia.
Other chemicals — including serotonin, acetylcholine and GABA — may also play a role. This may help explain why medications other than antipsychotics can sometimes cause tardive dyskinesia.
Tardive dyskinesia is most often a side effect of certain medications. These include:
In rare cases, tardive dyskinesia has also been linked to:
Doctors prescribe antipsychotic medications (neuroleptics) to treat conditions that involve psychosis, like schizophrenia. They also use them to treat depression, bipolar disorder, severe agitation and sometimes insomnia. These medications most often cause tardive dyskinesia.
First-generation (typical) antipsychotics cause tardive dyskinesia more often than second-generation (atypical) antipsychotics. However, almost any antipsychotic can cause TD. Clozapine and quetiapine carry a lower risk than most others.
Examples of first-generation antipsychotics include:
Metoclopramide is a medication that can relieve GERD (chronic acid reflux). It can also help treat diabetes-related gastroparesis.
Metoclopramide is strongly linked to TD. Risk factors for developing metoclopramide-induced TD include:
Antidepressants treat depression and other conditions like anxiety and obsessive-compulsive disorder.
Advertisement
Experts still debate whether antidepressants directly cause tardive dyskinesia. When TD happens in people taking antidepressants, it appears more often in adults over 65, possibly due to age-related brain changes. Overall, antidepressants cause TD much less often than antipsychotic medications.
Researchers have linked the following antidepressants to TD, although they aren’t sure whether the medication directly caused it:
Certain factors can increase your risk of developing tardive dyskinesia:
Advertisement
Researchers are also studying genetic factors that may increase or decrease your risk.
The uncontrollable movements of tardive dyskinesia can be uncomfortable and affect your social and emotional well-being. This can impact your mental health. It can also make it difficult to do everyday tasks.
TD generally isn’t fatal. But severe TD that affects your larynx (laryngospasm) and diaphragm can very rarely cause breathing issues that can be life-threatening.
Your healthcare provider will ask about your symptoms and review your medical and medication history. If you take a medication known to cause tardive dyskinesia, your provider may suspect TD. They’ll also do a physical exam and a neurological exam. In some cases, they may refer you to a specialist, like a neurologist, movement disorder specialist or psychiatrist.
Healthcare providers refer to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to diagnose tardive dyskinesia. According to these guidelines, symptoms must last at least one month after you stop the medication. You must also have taken the medication for at least three months if you’re 40 or younger, or at least one month if you’re over 40.
Advertisement
Your provider may order tests to rule out other conditions that cause similar symptoms, like Huntington’s disease. These tests may include lab work or imaging tests like a brain CT scan or MRI. But TD is usually a clinical diagnosis. This means your provider can often diagnose it based on your history and exam without additional testing.
Treatment for tardive dyskinesia varies. In some cases, symptoms improve when your provider lowers the dose of the antipsychotic medication or stops it. But symptoms can continue even after you stop the medication.
If possible, your provider may recommend stopping the medication that caused TD. However, this isn’t always an option because stopping it may worsen the condition it treats.
If you develop TD while taking a first-generation (typical) antipsychotic, your provider may switch you to a second-generation (atypical) medication. Clozapine and quetiapine carry a lower risk of causing or worsening TD than many other antipsychotics.
Medications called VMAT2 inhibitors offer the strongest evidence for treating TD. These include tetrabenazine, deutetrabenazine and valbenazine. Research shows these medications are safe and effective. Your provider may prescribe one if you have moderate to severe TD that affects your quality of life.
Providers may treat certain symptoms — like frequent eye blinking or muscle spasms in your neck, trunk or limbs — with botulinum toxin injections. If severe symptoms don’t improve with medication or injections, your provider may consider deep brain stimulation surgery in select cases.
Sometimes, symptoms improve or go away after you stop the medication that caused them — especially if you stop it early.
However, some cases become long-term (chronic). Medications can help manage symptoms, but they don’t always cure or reverse the condition.
Tardive dyskinesia affects everyone differently. The symptoms can range from mild to severe. In addition, treatment helps manage the symptoms for some but not for others. Your healthcare provider will work with you to find the best treatment plan. They’ll be able to give you a better idea of what to expect.
Tardive dyskinesia isn’t always preventable. Not everyone who takes certain medications develops it.
If you have risk factors, talk to your healthcare provider. They may prescribe a different medication to lower your risk. Providers also reduce risk by prescribing the lowest effective dose of an antipsychotic for the shortest time possible. They may choose medications that carry a lower risk of TD, such as quetiapine or clozapine.
If you need to take a medication known to cause TD, ask your provider about regular screenings for movement symptoms. Finding symptoms early may help reduce their severity. Most experts recommend screening every three to six months after you start a medication that can cause TD.
Your healthcare provider will work with you to adjust your treatment plan as needed. Other steps you can take to manage TD include:
If tardive dyskinesia is making it difficult to breathe, call 911 or go to the nearest emergency room as soon as possible.
Tardive dyskinesia (TD) affects everyone differently. For some, it can significantly affect their quality of life. Know that your healthcare provider will be by your side to monitor and manage TD. They can recommend and adapt treatment plans to fit your needs and suggest self-care strategies that can help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Parkinson’s disease, essential tremor and dystonia are common movement disorders. And Cleveland Clinic has the expert care and support you need to manage them.
