Blepharospasm is when uncontrollable muscle twitches or spasms force your eyelids closed. When it’s severe, the spasms can be enough to keep you from seeing. While this condition is rare, it’s also very disruptive. Fortunately, this condition is treatable, and several approaches can help.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
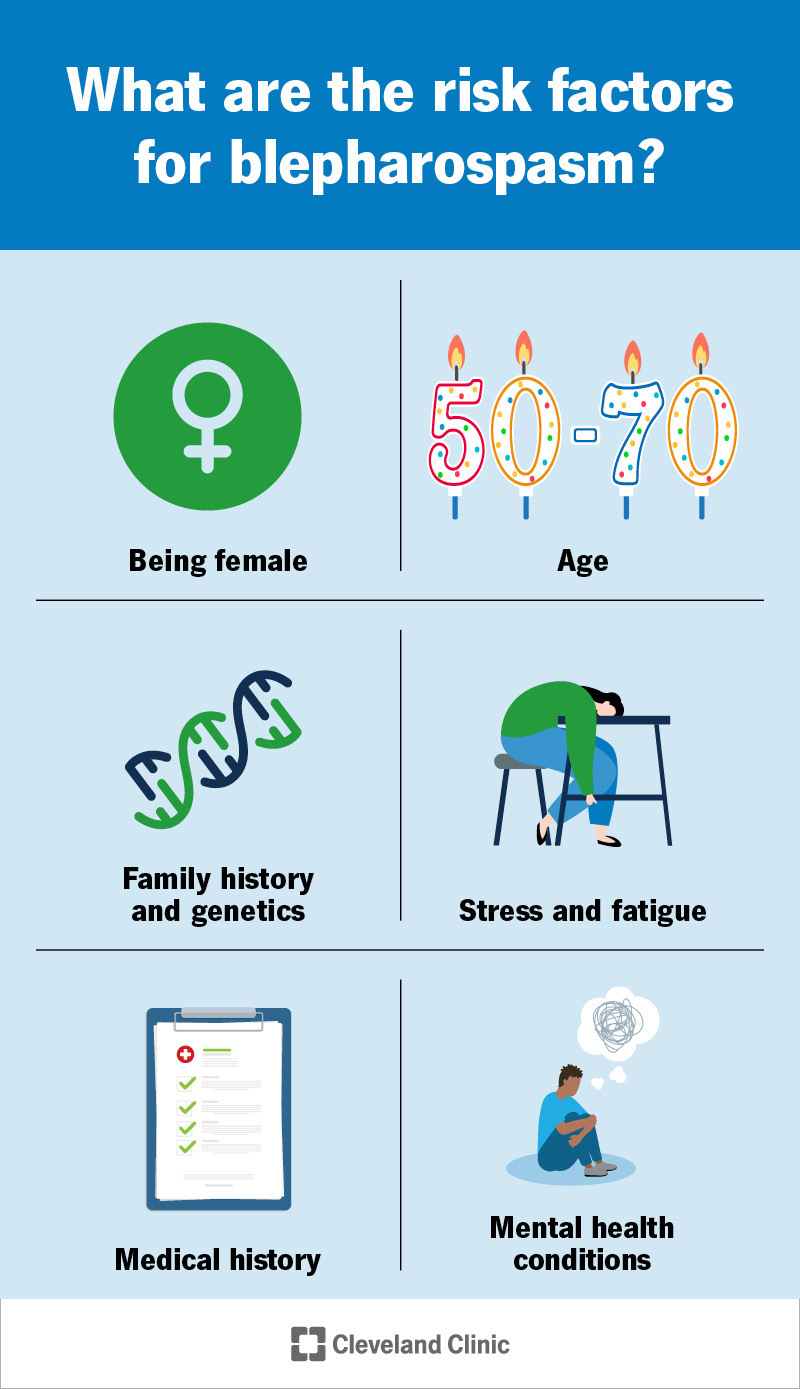
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21546-blepharospasm)
Blepharospasm is a type of eye twitching where the muscles in or around your eyes that open and close your eyes twitch or flex (spasm) rapidly and uncontrollably. In severe cases, the spasms can force your eyes shut, limiting your eyesight.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Research shows blepharospasm is mainly a neurological (nervous system-related) issue. Your eyes contribute to when and how the spasms happen.
There are two main ways that blepharospasm happens:
Experts aren’t sure just how common blepharospasm is. Based on available data, experts estimate there are 2,000 new cases of BEB diagnosed each year in the U.S. Estimates on how many people have it range between 5,000 and 100,000 in the U.S. and between 128,000 and 2.4 million worldwide.
Those estimates are broad for multiple reasons. One reason is that benign essential blepharospasm is difficult to detect, so many cases go undiagnosed. Secondary cases also may be undercounted because providers list another condition as the cause. Lastly, blepharospasm can — and often does — go away spontaneously.
Advertisement
Eyelid twitching is the only symptom of blepharospasm. But what sets it apart from other similar conditions are certain features or details of the spasms, or the way you blink your eyes. They include:
Experts suspect that blepharospasm happens because of issues involving one of the following:
BEB, the primary form of blepharospasm, is idiopathic, meaning it happens for reasons that experts don’t fully understand yet.
Secondary blepharospasm can happen with several possible causes or contributing factors. They include:
Advertisement
Several factors have links to blepharospasm, including:
Blepharospasm isn’t dangerous on its own, but it can be very disruptive or make ordinary situations hazardous. The spasms can make it hard to see or even force your eyes shut completely. When severe, the spasms can make it difficult or even impossible to drive, work, read and more.
Advertisement
Having blepharospasm can also contribute to significant stress and other mental health concerns. People who have blepharospasm commonly feel anxious or scared about the possibility of having a blepharospasm attack in public or around others. To avoid potential embarrassment or difficult situations, many people try to avoid situations where others might notice their condition, leading to issues like depression, anxiety and social isolation either developing or getting worse.
Blepharospasm is difficult to diagnose, and many people need to see multiple providers from different medical specialties, such as:
Diagnosing blepharospasm usually involves both a physical and neurological exam. One specific test that might help (but isn’t always necessary) is electromyography.
Other tests might be possible, depending on other conditions your provider suspects or your medical history. Your provider can tell you more about other tests they think might help.
Advertisement
Blepharospasm is often treatable, but there’s no way to cure it yet. The treatments can also range from simpler, noninvasive methods to surgery. When blepharospasm happens with a specific cause, treating that cause is often helpful. Cases may go away on their own, but that’s uncommon and experts aren’t certain why this happens (or if it really goes away for good).
The most common and effective treatments specifically for blepharospasm include:
OnabotulinumtoxinA is usually the first line of treatment for blepharospasm. Healthcare providers use it to weaken some of the muscles just enough to limit spasm-causing signals but not so much that you can’t blink your eyes.
These treatments usually involve four to eight injections with a tiny needle into the muscles around your eyes. The injections usually start working within two or three days and are usually effective for three to four months. But the effect isn’t permanent, so follow-up injections are almost always necessary. And some people may need larger doses as their bodies become used to the medication over time.
Filtering or blocking certain light wavelengths can reduce light sensitivity, which then helps blepharospasm. FL-41 is a specific pinkish tint that’s most effective. Glasses with these lenses are often called “blue light glasses” because they filter out blue wavelengths of light.
Glasses with FL-41 are usually available at places that specifically make or sell eyeglasses. You can also buy them online easily. And if you have prescription lenses, you might be able to get FL-41 lenses made with your prescription. Your eye care specialist can tell you more about whether that’s possible for your specific prescription.
Surgery is usually a last resort because it involves permanently thinning the muscle to weaken it. But for people with very severe blepharospasm that doesn’t respond to onabotulinumtoxinA injections, surgery may be the best option.
While it isn’t as common for treating blepharospasm, there’s research that indicates acupuncture can be an effective treatment. Your healthcare provider may be able to recommend accredited acupuncturists (including some who are also practicing medical doctors) who can help.
Blepharospasm isn’t life-threatening, but it can disrupt your usual routine and activities. The condition often starts with minor effects and gets worse over time. Eventually, the spasms are severe enough that they may prevent you from keeping your eyes open.
If you have questions about things that can help you adjust or compensate, your healthcare provider may be able to offer suggestions or guidance.
Primary blepharospasm is usually permanent. But some research studies show that it goes away spontaneously in about 11% of cases. More research is necessary to confirm that and explain how the condition can go away on its own.
Blepharospasm isn’t preventable, and there’s no known way to reduce your risk of developing it. But you may be able to reduce how often the symptoms happen or how severe they are.
Some things that might help include:
When blepharospasm is severe, you may need to make certain changes to your routine and activities. Some examples include:
There’s research that shows primary blepharospasm can go away spontaneously in some cases, but it’s not common. More research is necessary to confirm if it can go away and why it does. Secondary blepharospasm may go away with treatment of the underlying cause.
One small research study on 50 people from 2020 found that people with BEB were more likely to have lower levels of calcium and vitamin D, but that study didn’t specifically conclude that those deficiencies were causing blepharospasm. For now, there’s little to no research that conclusively shows blepharospasm can happen because of vitamin or mineral deficiencies.
Blepharospasm may be a rare condition that involves small, uncontrollable muscle movements, but it can have a big impact on your life. This condition can make it hard to do things you once had no problem doing, like driving a car, reading or watching TV. And if you can’t predict when spasms will happen or how they’ll affect you, it can make leaving your house a source of anxiety, worry or even fear.
If you think you have symptoms that could be blepharospasm, you should see an eye care specialist. They can either start the process of testing for this condition or guide you to a specialist who can. Treatment can make all the difference, keeping your eyes open and preventing this condition from shutting you out of all the things you’d rather be doing.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
