Overview
If you’ve been diagnosed with a human papillomavirus (HPV) infection or an abnormal Pap test, you aren’t alone. According to the Centers for Disease Control and Prevention, about 13 million Americans are newly diagnosed with HPV every year.
Sometimes HPV can lead to:
With advances in prevention, screening and management, we can prevent nearly all cervical cancers. In fact, the World Health Organization has issued a global call to eliminate cervical cancer.
Why Choose Cleveland Clinic?
- Industry leaders: Cleveland Clinic is a national leader and teaching hospital. We help our medical students, residents, and fellows learn how to manage abnormal Pap and HPV tests and intraepithelial neoplasia. We also teach and coach healthcare providers across the nation and worldwide through professional education seminars.
- Trusted experts: Our team of healthcare providers routinely meet to discuss difficult cases to make sure our patients receive the highest level of care.
- Collaborative care: We offer a convenient, team-based approach to manage abnormal Pap and HPV tests as soon as possible. Our evidence-based practices focus on cancer prevention, while preserving the cervix and uterus whenever possible.
- Specialized knowledge: Our specialists are experts at managing people at risk for cervical, vaginal and vulvar cancers. Sometimes abnormal cells that aren’t cancer grow on the surface of your cervix, vagina, or vulva. This is called intraepithelial neoplasia and having HPV puts you at higher risk for developing it. Some people with this condition develop cancer and some don’t. Our providers work with the gynecologic oncology team on complex cases.
- National recognition: Cleveland Clinic is recognized in the U.S. and throughout the world for its expertise and care.
Virtual visits
Want to get care without having to leave home? Virtual visits are a convenient and secure option that lets you talk to your provider from your smartphone, tablet or computer without needing to travel. We also understand that gynecologic care is highly personal and sometimes difficult to talk about. Our specialists will make sure you feel comfortable and have a positive experience at Cleveland Clinic.
Personalized care
We offer second opinions regarding diagnosis and treatment options to help our patients understand all of the treatment options available. Our team provides you with detailed information about treatment options and outcomes so you can make informed care decisions. This includes treatment for abnormal Pap or HPV tests and intraepithelial neoplasia. Diagnostic testing is done in the office or operating room by our staff providers.
What We Treat
Abnormal Pap or HPV Tests
The Center for Prevention of Cervical Cancer will complete a comprehensive evaluation to determine the cause of the abnormal test results and will work with you to determine the best treatment plan for you.
Abnormal Pap & HPV Tests
The Pap test is collected with a small plastic spatula and brush which collect cells from the cervix and/or vagina.
Learn more about what to expect during a Pap test.
Pap tests are generally classified as normal, inadequate (not enough cells to yield a reliable reading), or abnormal. An abnormal result can indicate that there is irritation to the cervix, or that the person may have a precancerous or cancerous lesion of the cervix.
The HPV test is run from the Pap sample and tests for 14 types of HPV known to cause cervical cancer. The Pap test and HPV test results are generally considered together to determine if the person needs additional testing.
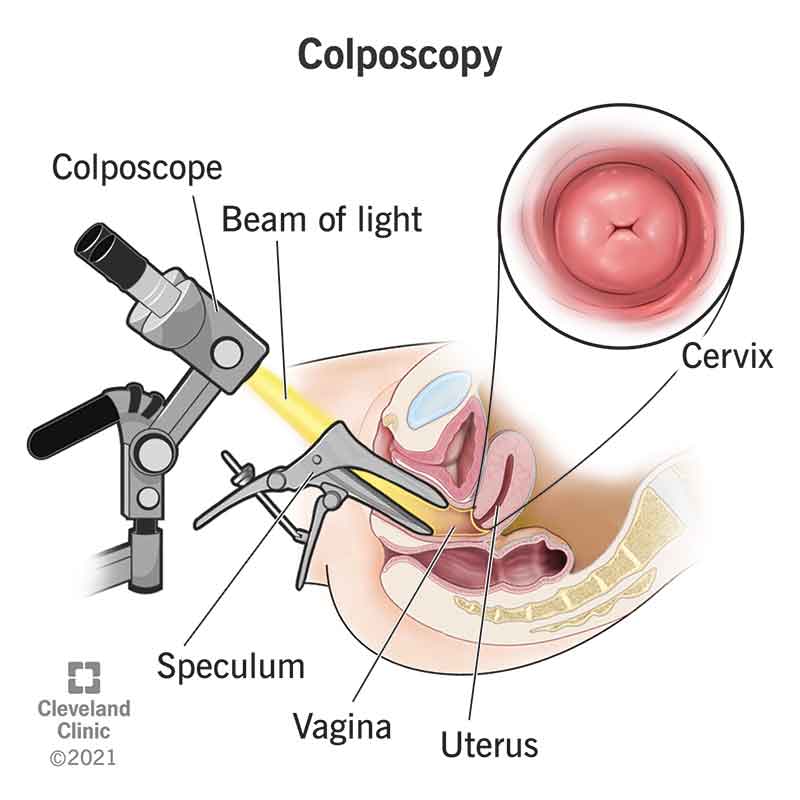
Colposcopy
A colposcopy is a procedure to check the cervix, the walls of the vagina and the vulva for signs of cancerous or pre-cancerous tissue. A colposcopy is usually performed to evaluate the cause of an abnormal Pap test, a positive HPV test or a vulvar lesion. A colposcopy may also be needed if there are abnormal lesions or vaginal bleeding.
During the procedure, a special lighted microscope, called a colposcope, magnifies the tissue that lines your cervix and vagina. Colposcopy also magnifies vulvar lesions when necessary. The physician will take tissue samples (biopsies) that can be tested in a lab for cancerous or precancerous cells. The biopsies taken at colposcopy are sent for pathologic evaluation and classification, which is required to guide proper treatment. The biopsies determine if there is CIN (cervical intraepithelial neoplasia), VAIN (vaginal intraepithelial neoplasia), and/or VIN (vulvar intraepithelial neoplasia, which are pre-cancerous lesions that require close observation or treatment.
CIN (Cervical Intraepithelial Neoplasia), also known as Cervical Dysplasia
Cervical dysplasia was once classified as mild, moderate or severe, based on how likely abnormal cells would become cancerous. A more recent system classifies disease severity based on how much epithelial tissue in your cervix has abnormal cells. Cervical intraepithelial neoplasia (CIN) is classified on a scale from one to three.
- CIN 1: Refers to abnormal cells affecting about one-third of the thickness of the epithelium.
- CIN 2: Refers to abnormal cells affecting about one-third to two-thirds of the epithelium.
- CIN 3: Refers to abnormal cells affecting more than two-thirds of the epithelium.
- CIN 1 cervical dysplasia rarely becomes cancer and often goes away on its own. CIN 2 and 3 are more likely to require treatment to prevent cancer.
VAIN (Vaginal Intraepithelial Neoplasia), also known as Vaginal Dysplasia
VAIN or vaginal dysplasia is diagnosed after biopsy of an abnormal area within the vaginal wall. VAIN is usually discovered during evaluation of an abnormal vaginal or cervical pap or HPV test. For most people who have had the cervix removed (most commonly done at hysterectomy), Pap and HPV tests are no longer necessary. For some, however, Pap and HPV tests should continue due to a history of high-grade precancerous lesions, cancer or symptoms such as vaginal bleeding after hysterectomy.
Like CIN, VAIN is caused by HPV infection and is similarly classified as VAIN 1, VAIN 2 and VAIN 3. VAIN 1 may resolve without treatment, while VAIN2 and VAIN 3 are more likely to require treatment to prevent cancer.
VIN (Vulvar Intraepithelial Neoplasia), also known as Vulvar Dysplasia
VIN or vulvar dysplasia is diagnosed after biopsy of an abnormal area in the skin of the vulva. VIN may present with changes in the skin color (more red, brown or white/pale than normal), a growth or lump, an open sore or rash that does not heal. VIN may be associated with itching or burning in the vulvar area that does not go away.
Like CIN and VAIN, VIN is commonly caused by HPV infection and is similarly classified as VIN 1, VIN 2 and VIN 3. VIN 1 may resolve without treatment, while VIN 2 and VIN 3 are more likely to require treatment to prevent cancer.
Learn more about VAIN, VIN and dysplasia of oropharynx, anus and penis.
Our Doctors
Looking for a cervical cancer prevention specialist?
Find a ProviderAppointments & Locations
Resources
Health Essentials:
Medical, health and wellness news, information and insights from Cleveland Clinic's experts.
Health Library:
Answers and details about popular health questions.