Penile cancer happens when healthy cells in your penis change and grow out of control. It’s rare in the U.S., but you should see your healthcare provider if you notice changes in your penis. Treatment in the early stages can keep the cancer from growing. Penile cancer that’s spread to other parts of your body is harder to treat.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
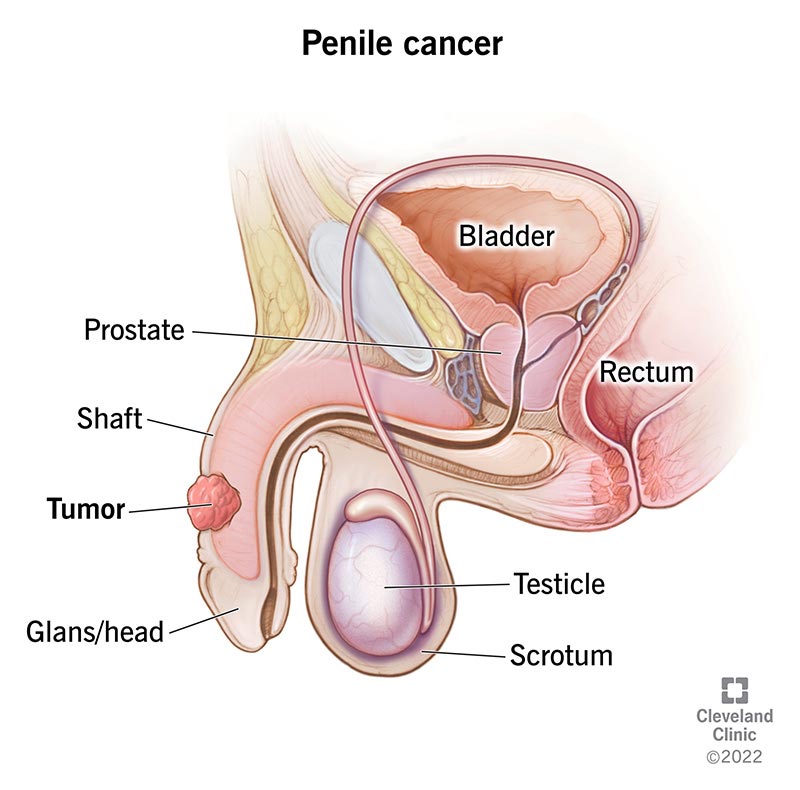
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/6181-penile-cancer)
Penile cancer develops when healthy cells in your penis change and grow out of control. Your penis is a rod-shaped reproductive organ that allows you to pee and have sex. Its main parts include the rod-like area (shaft) that extends from your low belly to the tip of your penis, called the head, or glans. If you’re uncircumcised, a layer of skin called the foreskin covers the head. If you’re circumcised, the head of your penis is exposed.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cancer can form anywhere in your penis, but it most commonly starts on the head or foreskin (if you’re uncircumcised).
Like many cancers, penile cancer is most treatable when diagnosed early. In many cases, it’s curable. If you notice something doesn’t seem quite right, tell a healthcare provider right away. Early detection is key.
Some types of penile cancer, listed from most to least common, include:
Advertisement
Penile cancer is rare in the United States, making up less than 1% of cancers among males. The condition is more common in Africa, Asia and South America.
Not all cancers cause changes you can see. But penile cancer usually causes your penis to look different. The skin on your penis may become discolored, and you may notice a lump.
Penile cancer symptoms include:
Less serious conditions like infections and allergic reactions also cause these symptoms. Still, don’t leave things to chance. It’s better to have a healthcare provider take a look so early-stage cancer doesn’t go untreated.
Cancer happens when healthy cells change and multiply out of control. But researchers don’t know what causes that change to begin with.
While researchers haven’t found causes, they’ve identified risk factors.
A risk factor doesn’t cause penile cancer, but it may increase the possibility. Penile cancer risk factors are:
A healthcare provider may do the following:
Treatment depends on the size of the tumor, whether it’s spread and how likely it is that the cancer will return (recur). Treatment may involve a care team that includes your primary care physician (PCP), a cancer specialist (oncologist), a urinary tract specialist (urologist), a radiation specialist (radiation oncologist) and a skin specialist (dermatologist).
For early-stage cancer, your healthcare provider may recommend one or more of the following treatments:
Advertisement
For cancer that’s more advanced, your healthcare provider may recommend:
Your healthcare provider may use radiation, chemotherapy or both before or after surgery.
For cancer that has spread outside of your lower belly, chemotherapy or other medicines (systemic treatment) are the main treatment.
Your chance of recovery and care plan depend on the following:
Catching cancer early means that it’s easier to treat and cure. Catching it later means there’s a greater chance that it’s spread beyond your penis. At this point, penile cancer becomes much harder to treat.
To reduce your risk of penile cancer, consider the following:
Advertisement
It’s important to consider the medical benefits of circumcision against other deciding factors, like religious beliefs and cultural and individual preferences. Talk through the benefits with your healthcare provider as you think about the best options for yourself or your newborn.
Talk to your healthcare provider about how your cancer diagnosis and treatment plan may impact your everyday life. Many cancer treatments preserve the penile tissue. This means that your penis eventually heals to look the same after treatment, or very similar, as it did before. You can still pee standing. You can still get an erection, have sex and orgasm.
Surgery to remove part or all of your penis may change the way you pee and your experience of sex.
Penile cancer and penile cancer treatment can unfold in various ways. Knowing what to expect can help you prepare for several potential scenarios. Speak openly with your healthcare provider about any questions you have.
Let your healthcare provider know if you develop new, changing or worsening symptoms. They can help determine whether cancer caused them.
If you have penile cancer, here are some questions you might want to ask your healthcare provider:
Advertisement
A penile cancer diagnosis is a life-changing event, stirring up a whirlwind of emotions and uncertainties. It’s OK (and natural) to feel overwhelmed, so it’s especially important to take good care of yourself right now. Talk to your healthcare provider. They can discuss potential treatment options and point you to resources for practical and emotional support. Lean on your medical team and loved ones. You’re not alone in this.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Penile cancer can be curable if caught early. Cleveland Clinic provides the diagnosis, treatment and support you need to keep enjoying life.
