Vulvar cancer is a rare cancer of your vulva. There are about 6,500 new cases of vulvar cancer in the U.S. each year. Most cases are related to either human papillomavirus (HPV) infection or lichen sclerosus. Changes in vulvar skin color and lumps or open sores may be signs of vulvar cancer. Treatments include surgery, radiation or chemotherapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
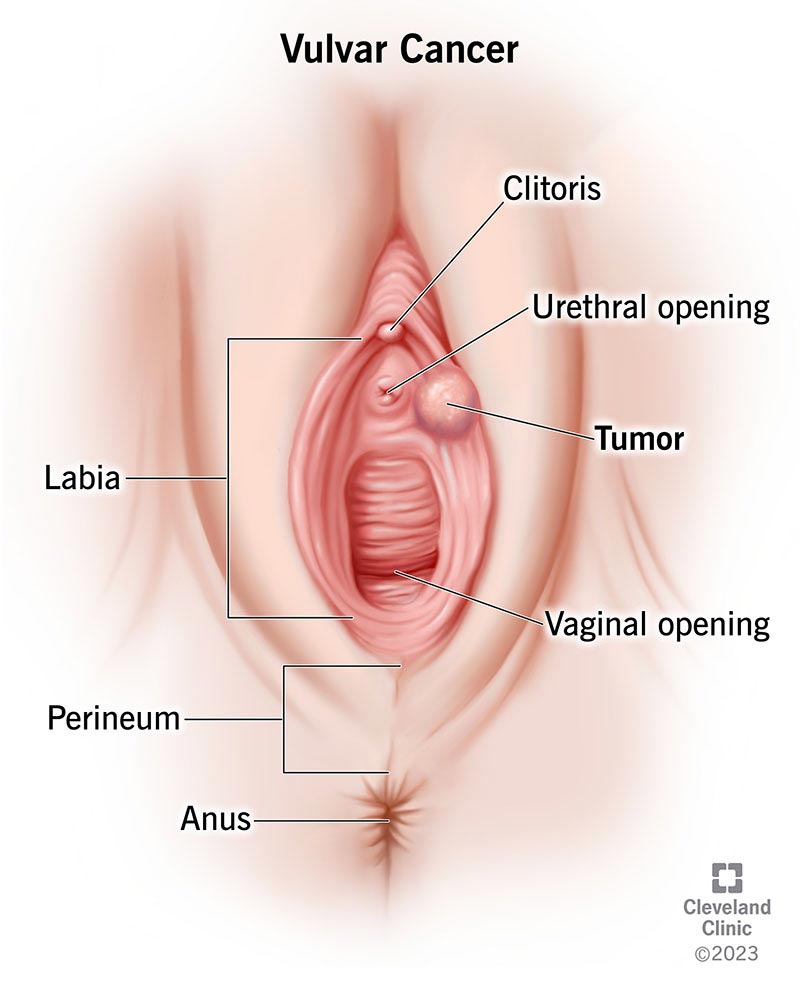
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/6220-vulvar-cancer)
Vulvar cancer is a rare cancer that forms in the tissues of your vulva. “Vulva” is the collective name for all the female external sex organs, or genitals. Your vulva includes:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Vulvar cancer usually develops slowly over several years. Precancerous areas of tissue (lesions) typically develop first. Healthcare providers usually discover the abnormal growth in the outermost layer of your skin. These precancerous lesions are called vulvar intraepithelial neoplasia (VIN).
Healthcare providers classify vulvar cancer based on the type of cells where the cancer starts. The most common types of vulvar cancer include:
Advertisement
The remaining vulvar cancers are rare. They include:
Vulvar cancer is rare. Healthcare providers diagnose just under 6,500 new cases of vulvar cancer in the U.S. each year.
Nearly 80% of people diagnosed are over age 50, and over half of all diagnoses are in people over age 70. The average age at diagnosis is 68.
The first noticeable signs of vulvar cancer are usually skin changes on your outer lips (labia majora) or inner lips (labia minora). But cancer can form anywhere on your vulva.
Vulvar cancer symptoms include:
See your healthcare provider if you have one or more of these symptoms. Vulvar cancer symptoms usually don’t appear in the early stages, so it’s important to get checked as soon as possible.
Still, many of these symptoms are also common in noncancerous conditions. Your provider can tell you whether these changes are signs of vulvar cancer or a different condition.
With vulvar cancer, cells begin multiplying out of control. Without treatment, these cancer cells can spread to other parts of your body.
The most common type of vulvar cancer, vulvar squamous cell carcinoma, arises in association with one of two conditions:
Risk factors for vulvar cancer include:
Advertisement
Your healthcare provider will ask about your medical history, potential risk factors and symptoms. Diagnosis often involves multiple tests.
Tests may include:
If you have cancer, your provider will perform additional tests to see if it’s spread beyond your vulva. Without treatment, vulvar cancer may spread to your vagina or other nearby organs, lymph nodes in your pelvis and eventually your bloodstream. Cancer that’s spread (metastatic cancer) is harder to treat.
Advertisement
Tests may include:
Vulvar cancer staging allows healthcare providers to determine if your cancer’s spread beyond your vulva. This information guides treatment decisions. There are four main stages:
Advertisement
Ask your healthcare provider to explain the details of what your cancer stage means for your treatment.
Your treatment depends on factors like your general health, cancer stage and whether your healthcare provider recently diagnosed your cancer or if it’s recurred (come back). Your provider can explain how your treatment plan is best suited for your diagnosis.
Surgery is the most common treatment for cancer of the vulva. The goal is to remove all the cancer while preserving your sexual function. Types of surgery include:
Radiation therapy uses X-rays or other high-energy sources to kill cancer cells. The most common delivery method for vulvar cancer treatment is external beam radiation therapy (EBRT). EBRT uses a machine to deliver radiation through your skin to the targeted cancer site.
Often, people receive radiation therapy and chemotherapy together (chemoradiation). You may receive radiation before surgery to shrink a tumor or after surgery to destroy any remaining cancer cells.
Chemotherapy uses drugs to attack cancer cells throughout your body. Your healthcare provider may inject the medicine into a vein or muscle, or you may take a pill. You may receive a lotion that you can apply directly to your vulva. This form of chemotherapy attacks cancer more locally — in the specific area.
Cisplatin (Platinol®, Platinol -AQ®) and fluorouracil (Carac®) are commonly prescribed chemotherapy drugs for vulvar cancer.
Immunotherapy helps your body’s immune system identify cancer cells and fight them more effectively. Imiquimod cream (Aldara®, Zyclara®) is a common immunotherapy medication used to treat vulvar cancer.
Your healthcare provider may perform tests at various checkpoints after treatment to monitor your condition and ensure the cancer hasn’t returned.
Testing often involves the same procedures used to diagnose and stage vulvar cancer.
It can be. Untreated vulvar cancer is life-threatening. Cancer that’s spread to your lymph nodes or other body parts is much harder to treat than cancer diagnosed early.
While there’s always a risk that cancer may return after treatment (recur), most people who receive treatment in the early stages of the disease remain cancer-free.
The relative five-year survival rate for people with vulvar cancer is approximately 70%. But survival rates are higher when people are diagnosed and treated in the early stages. For example, the five-year survival rate for localized cancer (remaining in the vulva) is approximately 86%. The five-year survival rate drops to approximately 30% once the cancer spreads.
Still, your prognosis depends on factors unique to your diagnosis, including your health and your response to treatment. Ask your healthcare provider about likely outcomes based on your diagnosis.
Most types of vulvar cancer progress slowly over several years. Less common types, like melanomas, tend to grow and spread more quickly.
The best way to reduce your risk is to get the HPV vaccine to prevent infections. In the U.S., adults up to age 45 may receive Gardasil 9® depending on their risk of HPV exposure. Cervarix® and Gardasil® are HPV vaccines available in other countries.
See your healthcare provider right away if you develop any symptoms of vulvar cancer. Schedule regular checkups, including a physical exam, at least annually for your gynecological health.
Many people feel self-conscious about visible changes to their vulva. Still, having vulvar cancer doesn’t mean you must abandon physical intimacy. Don’t be ashamed to ask your healthcare provider how your diagnosis may affect your sex life. They can connect you with resources that support your physical and emotional needs as you navigate your diagnosis and treatment.
Vulvar cancer usually starts on the surface of the skin surrounding your vagina, either your outer lips (labia majora) or inner lips (labia minora). Less commonly, it forms on other parts of your vulva, like your Bartholin gland and clitoris.
Stage I is the first stage of vulvar cancer. In this stage, cancer hasn’t spread beyond your vulva or perineum. Stage IA vulvar cancer is two centimeters (peanut size) or smaller. It hasn’t spread beyond one millimeter (tip of a pencil-size) into nearby tissue beyond one millimeter. Stage IB vulvar cancers involve larger tumors that may have invaded more deeply into nearby tissue.
You play a large role in your health. Become familiar with all parts of your body, including your vulva. Knowing what you look like now can help you easily identify changes. And when you see changes, make an appointment to see your healthcare provider. In the meantime, don’t skip visits to your gynecologist. They can identify precancerous changes before they become more serious.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vulvar cancer is rare and often complex. At Cleveland Clinic, we can diagnose and treat this condition and support you through your recovery.
