A colposcopy can check for precancerous or cancerous cells. Your healthcare provider may recommend one if you have abnormal Pap or HPV test results. You may be nervous about needing this procedure. But learning about the process and going over your pain management options may help relieve anxiety.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
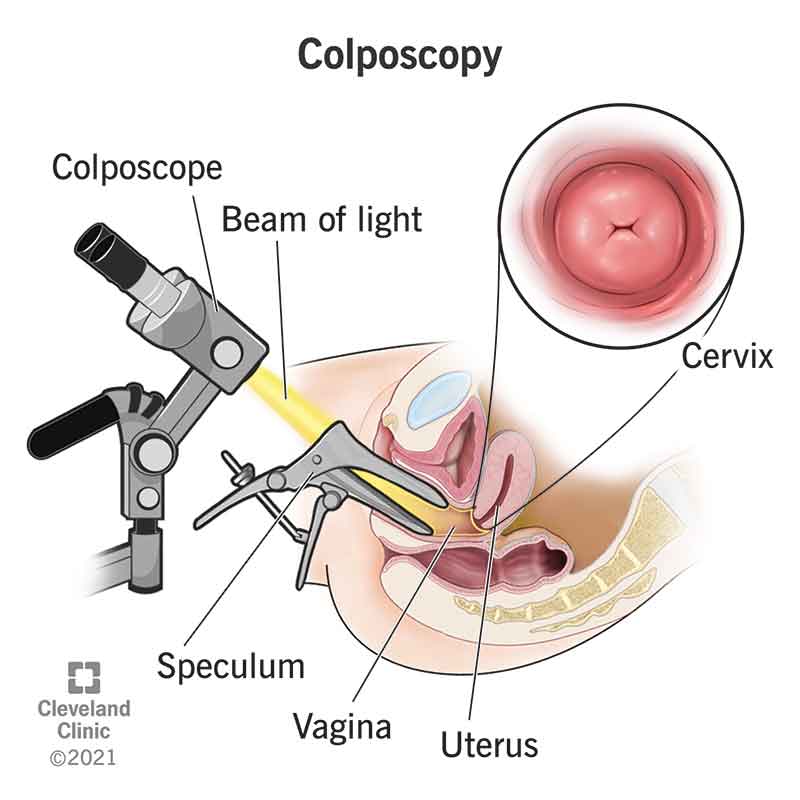
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4044-colposcopy)
Colposcopy is a procedure to check your cervix, vagina and vulva for abnormal tissue.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your healthcare provider will use a special tool called a colposcope. It has a bright light and works like a microscope to make the area look bigger. This helps them see the cells in the area more clearly.
If your provider finds anything that doesn’t look normal, they can take a small piece of tissue (called a biopsy). They’ll send the tissue sample to a lab to be checked.
A colposcopy mainly looks for cells that could turn into cancer (called cervical dysplasia). It can also test for genital warts and growths called cervical polyps.
You may need a colposcopy if you:
A colposcope has a built-in light and binocular-like lenses. It makes it easy for your provider to view your cervix while remaining seated at your feet. The colposcope remains outside your vagina the whole time.
If your healthcare provider sees abnormal cells through the colposcope, they take a biopsy. This is typically a punch biopsy or an endocervical curettage (ECC).
A punch biopsy removes a circular piece of tissue. Your provider uses a specialized tool that has a circular scalpel on the end. They remove the sample in one movement.
Advertisement
With an ECC, your provider scrapes the lining of your cervix with a spoon-shaped tool.
Your healthcare provider will tell you how to prepare for a colposcopy. In general, you should:
During a colposcopy, you can generally expect the following steps:
You can get a colposcopy in a medical office or clinic. It usually lasts 10 to 20 minutes. You should be able to go home the same day.
Everyone experiences pain differently. So, it’s impossible to predict how painful a colposcopy procedure will be for you. Various parts of the procedure may cause pain, including:
Before the procedure, talk to your healthcare provider about your pain management options. Taking an over-the-counter (OTC) pain reliever before it can help. Your provider may also offer a local anesthetic injection or a topical lidocaine spray. In rare cases, general anesthesia may be an option.
A colposcopy procedure is generally safe and low risk. But it can sometimes cause significant bleeding or an infection. These complications are treatable.
It can take a few days for your cervix to heal if you had a biopsy. You might experience:
Advertisement
You can use pads to manage any vaginal discharge or bleeding. Allow your cervix time to heal. Don’t insert anything into your vagina. Avoid penetrative sex and tampons. Ask your provider about how long you should avoid these things to ensure enough recovery time.
If you didn’t have a biopsy, you should be able to go back to your normal activities after the procedure. You may have mild spotting for a few days.
Biopsy results usually arrive within two to 10 days. Ask your provider about when you should expect results and how you’ll learn about them.
You’ll get a normal or abnormal result from your colposcopy.
A normal result means the biopsy didn’t show any abnormal cells. This means you don’t need treatment. But you’ll still need routine cervical cancer screening. Your healthcare provider will let you know how often to get it.
An abnormal result means the biopsy showed abnormal cells. This means you’ll likely need treatment or close monitoring. If you get an abnormal result, it’s typically precancerous cells. In rare cases, a colposcopy can lead to a cervical cancer diagnosis.
Your healthcare provider will explain the next steps in detail. They depend on the type and severity of the abnormal cells.
Advertisement
If the results reveal mild cervical dysplasia, your provider will ask you to repeat the Pap test periodically. Mild dysplasia may go away on its own (tissue returns to normal without treatment).
Treatments for more advanced precancerous cells include:
If you have cervical cancer, you’ll meet with a team of healthcare providers to figure out your treatment plan.
Colposcopy is a relatively safe procedure with few side effects. But you should call your provider if you notice any of the following symptoms:
Hearing you need a colposcopy may cause anxiety and distress. But know that this procedure is very important. It can help your healthcare provider identify any cancer or precancerous cells early so that you get the treatment you need. And the sooner you can get treatment (if you need it), the better.
Don’t hesitate to ask your healthcare provider about the details of a colposcopy and how to manage pain. The more you know about what to expect, the more comfortable you may feel going into the procedure.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From routine pelvic exams to high-risk pregnancies, Cleveland Clinic’s Ob/Gyns are here for you at any point in life.
