Neuroimmunology - Cleveland

The neuroimmunology training program at the Cleveland Clinic Mellen Center comprises two fellowships:
- Neuroimmunology Fellowship (1-year clinical).
- Neuroimmunology – Clinical and Research Fellowship (2-year clinical and research).
The fellowships are designed to prepare academically oriented adult neurologists, pediatric neurologists, and physiatrists for a career in patient care and clinical research in multiple sclerosis (MS) and other autoimmune neurologic disorders. The Neuroimmunology Fellowship is a 1-year program focusing on clinical training. The Neuroimmunology – Clinical and Research Fellowship is a 2-year program which combines clinical and research training. By mutual agreement of the Fellow and program, the duration of each can be extended. To be eligible, applicants are required to have completed a residency (or international equivalent specialty training) in Adult Neurology, Pediatric Neurology, or Physical Medicine and Rehabilitation and must be eligible for an Ohio medical or training license (ECFMG certification if international). International applicants are welcome, and visa sponsorship is possible.
Unique aspects of the Fellowships:
- Well-developed curriculum with the flexibility to tailor focus of the training program to the Fellow’s background, interests, and career goals.
- Established track record of successfully training more than 50 clinical fellows. We usually have 4-6 Fellows at a given time and offer 2-5 new positions per year.
- Hands-on teaching from a large, engaged, expert faculty.
- Participation of the Fellow in the on-site multidisciplinary team that provides comprehensive care to a large number of adults and children with MS and other autoimmune disorders.
- Opportunity to participate in an active clinical research program that includes clinical trials and a wide variety of other research studies.
Overview of the Mellen Center
The Mellen Center, directed by Dr. Robert Bermel, is a comprehensive MS and autoimmune neurology program providing clinical care and conducting research within the Cleveland Clinic Neurological Institute. The Mellen Center is among the largest clinical neuroimmunology programs worldwide, with 1000-2000 new patients yearly and more than 25,000 total visits annually. The total currently active patient base is approximately 14,000. Mellen Center physician staff includes 17 neurologists who specialize in MS and other autoimmune neurologic disorders (Justin Abbatemarco, MD, Aaron Abrams, MD; Moein Amin, MD MSc; Robert Bermel, MD MBA; Adrienne Boissy, MD MS; Alise Carlson, MD MSc; Jeffrey Cohen, MD; Devon Conway, MD MSc; Kimberly DiMauro, DO; Robert Fox, MD MSc; Amy Kunchok, MD PhD; Kedar Mahajan, MD PhD; Marisa McGinley, DO MSc; Brandon Moss, MD MSc; Daniel Ontaneda, MD PhD; Mary Rensel, MD; and Lindsay Ross MD MSc), including 3 staff neurologists with fellowship training in Autoimmune Neurology and 1 staff neurologist with fellowship training in Pediatric Neuroimmunology. There are 6 physiatrists (Francois Bethoux, MD; Geraldine Dapul, MD; Juliet Hou, MD; Branden King, DO; Keith McKee, MD; and Eileen Slavin, DO). There are 3 Neuroradiologists in the Mellen Center with a special interest in demyelinating disease (Steven Jones, MD PhD; Chintan Shah, MD; and Emmanuel Obusez, MD). Non-physician staff includes advanced practice clinicians, nurse care coordinators, infusion nurses, medical assistants, social workers, health psychologists, cognitive psychologists, psychology fellows, neuropsychology technicians, physical/occupational/speech therapists, and administrative support staff.
Clinical visits cover diagnostic questions, confirmation of the diagnosis of MS and other autoimmune neurologic disorders, disease management recommendations and implementation, symptom management recommendations and implementation, and evaluation for potential participation in clinical trials and other research studies including cell-based therapies. Clinical visits are supplemented by quantitative neuroperformance testing and patient reported outcomes for all visits. Specialized programs include outpatient parenteral drug administration, multidisciplinary symptom management programs, a comprehensive Mellen rehabilitation program, Health Psychology, Neuropsychology, Autoimmune Neurology, and Pediatric Neuroimmunology.

The Mellen Center is fully accessible to individuals with disabilities and has areas for appointment scheduling, financial counseling, patient education, rehabilitation therapies, individual and group health psychology visits, neuropsychological testing, 16 medical exam rooms, 2 procedures rooms, 15-chair infusion center, work area for specimen preparation and storage, conference rooms, and office space. There is a unique clinical intake space for 9 patients to perform technology-enabled neuroperformance testing and complete patient-reported outcome questionnaires on computer tablets with the results uploaded immediately to the electronic medical record for patient care and registry for research. This testing has been fully integrated into routine visit flow. The Mellen Center is located in close proximity to Adult and Pediatric Neurology, the main Cleveland Clinic, and the Lerner Research Institute (which houses collaborators in Quantitative Health Sciences, Neuroscience, Immunology, and Biomedical Engineering). Case Western Reserve University and Medical Center (collaborators and graduate courses) is 5 minutes away by car.
The Mellen Research Program, directed by Dr. Daniel Ontaneda (Fellowship Associate Director) includes 4 research nurses, 8 research coordinators, 2 research supervisors, 1 recruitment coordinator, 1 program manager, 3 project managers, a data manager, a master’s level statistician, a PhD level statistician, and administrators. All of the Mellen Center professional staff members participate in clinical trials and other clinical research projects (as PI or Co-Investigator).
The Mellen Imaging Center directed by Dr. Stephen Jones (Department of Radiology) houses 3 3 tesla scanners (Siemens Skyra®, Siemens Prisma Fit®, Magneton Cima.X®), one mock scanner (0T), and a 7 tesla clinical/research scanner (Siemens Terra®), including dedicated brain, cervical spine, and whole spine coils. There are numerous workstations running image processing software to register images; quantify lesions; quantify whole brain, regional, and white and gray matter atrophy; cortical thickness; and spinal cord cross-sectional area. Dr. Stephen Rao directs the Schey Center for Cognitive Neuroimaging that studies fMRI in MS and other neurodegenerative diseases. The Mellen Center Optical Coherence Tomography laboratory directed by Dr. Robert Bermel houses a Zeiss Cirrus spectral domain OCT machine. The Mellen Gait and Balance Analysis Laboratory is equipped with a GAITRite gait analysis system, Tetrax computerized balance testing platform, exoskeleton walking device (EksoGTTM), and CAREN system (a state-of-the-art fully immersive virtual reality and motion analysis system).

The Mellen Center Registry contains comprehensive data on nearly 10,000 patients with up to 8 years of follow-up, including demographics, disease characteristics, geographic information related to access to care, neuroperformance testing, patient-reported outcomes of quality of life and disability, quantitative MRI analyses (lesion volumes, brain volume, regional brain volumes, and spinal cord cross-sectional area), and OCT metrics.
These resources are available to Fellows for clinical care and research projects.
Components of the Training Program
Patient Care
One aspect of fellowship training is supervised patient care to develop specialized expertise in the diagnosis and management of MS and other autoimmune neurological disorders. The Mellen Center has emphasized multidisciplinary care since the program was founded in the 1980s. Fellows participate as active members of the multi-disciplinary team that evaluates and treats a large number of patients (we are among the largest neuroimmunology programs worldwide). Fellows see both new patients and established patients in their own follow-up practice. Fellows also have the opportunity to get hands-on experience with spasticity treatment (botulinum toxin injection and intrathecal baclofen pump management) and performing and interpreting OCT.
The relative proportions of time spent seeing MS versus autoimmune neurology can be tailored to the fellow’s interests. It also is possible to pursue a training program with greater emphasis on pediatric or rehabilitative aspects of MS and other autoimmune neurologic disorders.
Autoimmune Neurology
The autoimmune neurology program is directed by Dr. Amy Kunchok (Fellowship Associate Director). We see a large number of patients with autoimmune neurological disorders in the clinic and for subspecialty consultations at the Main campus hospital. Our clinical population includes approximately 300 people with NMOSD, 130 with MOGAD, 50 with NMDAR autoimmune encephalitis, 50 with LGI1 autoimmune encephalitis, 100 with paraneoplastic neurological disorders (ANNA1/Hu, CRMP5/CV2, ma1/ma2, KLCH11, PCA1/Yo), and various other neural antibody mediated disorders (IgLON5, DPPX, GABA-B-R, GAD65, Glycine-R, Septin-5, CASRP2, GFAP, etc.). Additionally, we manage ~200 patients with neurosarcoidosis (led by Dr. Brandon Moss) in clinical collaboration with the multidisciplinary sarcoidosis clinic (with Pulmonology, Cardiology and Rheumatology). We also consult on patients with neurological autoimmunity in the setting of immune checkpoint inhibitors (immune related adverse events, (irAE)) and are part of a multidisciplinary irAE clinician group with the Oncology Institute and collaborate in caring for these patients.
Research in autoimmune neurology is predominantly clinical with opportunities to focus on clinical phenotyping, clinical outcomes, barriers to care, MRI (including advanced MRI techniques), and PET imaging. We have clinical and imaging databases for these purposes. We have laboratory collaborations with the immune-oncology laboratory for biomarker research and a biorepository of blood and CSF samples from autoimmune neurology patients. We are running several clinical trials in autoimmune neurology for novel therapeutics.
All Fellows receive training in MS and other autoimmune neurologic disorders. It is possible to pursue a training program focusing on Autoimmune Neurology.
Pediatric Neuroimmunology
The Pediatric MS and Neuroimmunology Program is co-directed by Dr. Aaron Abrams (Pediatric Neurology and Mellen Center) and Dr. Mary Rensel (Mellen Center). The Cleveland Clinic is recognized as a Center of Excellence by the National MS Society and is represented on the Steering Committee of the US Network of Pediatric MS Centers, a national consortium dedicated to improving the lives of children and families affected by neuroimmunologic conditions through collaboration in professional, academic, and research initiatives.
All Fellows rotate through the Pediatric MS and Neuroimmunology Program to enhance their understanding of pediatric-onset MS and other autoimmune neurologic conditions, such as NMOSD, MOGAD, autoimmune encephalitis, neurosarcoidosis, and CNS vasculitis in children and adolescents. We also offer specialized training programs within the Neuroimmunology Fellowship and Neuroimmunology – Clinical and Research Fellowship for those interested in focusing on pediatric neuroimmunology.
Rehabilitation
Fellows have access to advanced neurorehabilitation services within the Mellen Center, including symptom management (e.g., bladder, bowel, spasticity, tremor, pain, and fatigue), cognitive rehabilitation, power mobility assessment, and virtual reality rehabilitation. The neurorehabilitation team comprises 6 physiatrists (Drs. Francois Bethoux, Keith McKee, Geraldine Dapul, Juliet Hou, Eileen Slavin, and Branden King), advanced practice clinicians, nurses, and physical, occupational, and speech therapists. The on-site gym is equipped with state-of-the-art rehabilitation technology such as a robotic exoskeleton, motion analysis- and virtual reality-augmented treadmills (C-Mill and CAREN system). The Mellen Center also hosts a busy spasticity clinic, with multiple training opportunities in therapeutic procedures, including botulinum toxin and phenol injections, and intrathecal baclofen therapy. Participation in rehabilitation research projects is also available, with a particular emphasis on spasticity, exercise, and motion analysis for gait/balance disorders associated with MS and other autoimmune neurologic disorders.
As members of the multidisciplinary care team, all Fellows receive training in rehabilitation as it relates to MS and other autoimmune neurologic disorders. It is possible to pursue a training program focusing on neuroimmunologic rehabilitation.

Imaging
Training in MRI is obtained through interpreting studies as part routine patient care and several case conferences (managed by the Fellows) in which studies are reviewed with Neuroradiology. Dedicated research imaging training is conducted within the Mellen Imaging laboratory directed by Dr. Kunio Nakamura (Lerner Research Institute). Fellows also are trained to perform and interpret OCT. Research projects utilizing conventional MRI, advanced MRI, or OCT are possible.
Clinical Trials
We participate in a large number of clinical trials, and Mellen Center staff members often fill leadership positions in those trials. All Fellows participate as a co-investigator in ongoing trials. Fellows serve as an Examining Physician to develop expertise in a standardized neurologic examination, calculating rating scales such as the NeuroStatus EDSS, and performing the MS Functional Composite. In other trials, Fellows serve as Treating Physician to become familiar with issues involved in patient management within the constraints of a protocol. Fellows gain experience in trial management and implementation by serving as the de facto Site Principal Investigator for a clinical trial under staff supervision. Responsibilities include composing the consent form, preparing the IRB application, reviewing the budget, coordinating contract negotiation, managing regulatory documents, supervising patient recruitment, planning study visits, developing source documents, and working with data coordinators and study monitors to resolve queries.
Graduate Coursework
We encourage and help arrange coursework in, for example, statistics, epidemiology, and trial design. Most Fellows in the 2-year Neuroimmunology – Clinical and Research Fellowship complete the requirements for a Master’s Degree or PhD at Case Western Reserve University. Potential areas of focus include Experimental Therapeutics, Imaging, Epidemiology, Bioinformatics, and Statistics in MS or other autoimmune disorders.
Clinical Research
All fellows engage in some research. Although research is not an emphasis of the 1-year clinical program, those Fellows prepare at least one manuscript for publication, participate as a co-investigator in clinical trials to gain some exposure to clinical trial conduct, and carry out focused research projects.
Fellows pursuing clinical research training and a Master’s Degree or PhD design, carry out, analyze, and report a formal independent research project to fulfill the requirements. For this, graduate school faculty and members of the Mellen Center staff serve as mentors. The project is designed during the first year and carried out during Years 2-3. This experience familiarizes the Fellow with formulating a research question, designing and carrying out a clinical experiment, and analyzing and interpreting the results.
Basic and Translational Science Research
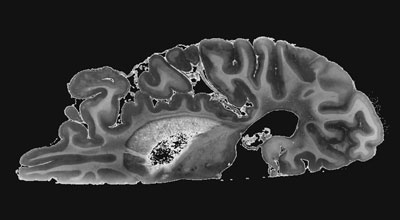
Fellows interested in pursuing career in basic and translational science can conduct research at the Lerner Research Institute Department of Neurosciences led by Dr. Bruce Trapp. Research is mainly focused on the Mellen Center Brain Donation program which contains brains and spinal cords of 200 cases of MS. Research projects can be conducted in MRI-pathology correlation studies, myelination, CNS immune regulation, glial biology, blood brain barrier dysfunction, viral CNS infections, CNS meninges, among other topics.
Didactic and Scholarly Activities
To supplement the clinical and research activities described above, there is a weekly lecture series, monthly journal club, weekly Mellen Center case conference, every other month Autoimmune Neurology case conference, quarterly multi-institutional international MRI case conference, monthly Mellen Approaches conference, and monthly Mellen research conference, plus a variety of other clinical and research conferences. Fellows are encouraged to prepare abstracts and present at meetings. They have the opportunity to author or contribute to review articles, chapters, and primary publications.
Selected Publications
- Rudick RA, Cohen JA, Weinstock-Guttman B, Kinkel RP, Ransohoff RM. Management of multiple sclerosis. N Engl J Med 1997;337(22):1604-11. PMID: 9371858
- Bermel RA, Bakshi R. The measurement and clinical relevance of brain atrophy in multiple sclerosis. Lancet Neurol 2006;5(2):158-70. PMID: 16426992
- Cohen JA, Barkhof F, Comi G, Hartung H-P, Khatri BO, Montalban X, Pelletier J, Capra R, Gallo P, Izquierdo G, Tiel-Wilck K, de Vera A, Jin J, Stites T, Wu S, Aradhye S, Kappos L, for the TRANSFORMS Study Group. Oral fingolimod or intramuscular interferon in relapsing multiple sclerosis. N Engl J Med 2010;362:402-15. PMID: 20089954 DOI: 10.1056/NEJMoa0907839
- Cohen JA, Reingold SC, Polman CH, Wolinsky JS, on behalf of the International Advisory Committee on Clinical Trials in Multiple Sclerosis. Disability outcomes in multiple sclerosis clinical trials: current status and future prospects. Lancet Neurol 2012;11:467-76. PMID: 22516081 DOI: 10.1016/S1474-4422(12)70059-5
- Cohen JA, Coles AJ, Arnold DL, Confavreux C, Fox EJ, Hartung HP, Havrdova E, Selmaj KW, Weiner HL, Fisher E, Brinar VV, Giovannoni G, Stojanovic M, Ertik BI, Lake SL, Margolin DH, Panzara M, Compston DAS, for the CARE-MS I investigators. Alemtuzumab versus interferon beta as first-line treatment for patients with relapsing-remitting multiple sclerosis: a randomised controlled phase 3 trial. Lancet 2012;380:1819-28. PMID: 23122652 DOI: 10.1016/S0140-6736(12)61769-3
- Fox RJ, Miller DH, Phillips JT, Hutchinson M, Havrdova E, Kita M, Yang M, Raghupathi K, Novas M, Sweetser MT, Viglietta V, Dawson KT; CONFIRM Study Investigators. Placebo-controlled phase 3 study of oral BG-12 or glatiramer in multiple sclerosis. N Engl J Med 2012;367(12):1087-97. PMID: 22992072
- Bermel RA, You X, Foulds P, Hyde R, Simon JH, Fisher E, Rudick RA. Predictors of long-term outcome in multiple sclerosis patients treated with interferon β. Ann Neurol 2013;73(1):95-103. PMID: 23378325
- Cohen JA, Krishnan AV, Goodman AD, Potts J, Wang P, Havrdova E, Polman C, Rudick RA. The clinical meaning of walking speed as measured by the timed 25-foot walk in patients with multiple sclerosis. JAMA Neurol 2014;71:1386-93. PMID: 25178496 DOI: 10.1001/jamaneurol.2014.1895
- Cohen JA, Belova A, Selmaj K, Wolf C, Oberyé J, van den Tweel E, PhD, Mulder R, Koper N, Voortman G, Barkhof F, for the GATE Study Group. Equivalence of generic glatiramer acetate in multiple sclerosis. JAMA Neurol 2015;72:1433-41 DOI: 10.1001/jamaneurol.2015.2154 PMID: 26458034
- Ontaneda D, Fox RJ, Chataway J. Clinical trials in progressive multiple sclerosis: lessons learned and future perspectives. Lancet Neurol 2015;14(2):208-23. PMID: 25772899
- Scolding NJ, Pasquini M, Reingold SC, Cohen JA. Cell-based therapeutic strategies for multiple sclerosis. Brain 2017 Jul 21;140(11):2776–2796. doi: 10.1093/brain/awx154
- Ontaneda D, Thompson AJ, Fox RJ, Cohen JA. Progressive multiple sclerosis: prospects for disease therapy, repair, and restoration of function. Lancet 2017;389(10076):1357-66. PMID: 27889191 DOI: 10.1016/S0140-6736(16)31320-4
- Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, Correale J, Fazekas F, Filippi M, Freedman MS, Fujihara K, Galetta SL, Hartung HP, Kappos L, Lublin FD, Marrie RA, Miller AE, Miller DH, Montalban X, Mowry EM, Soelberg-Sorensen P, Tintoré M, Traboulsee AL, Trojano M, Uitdehaag BMJ, Vukusic S, Waubant E, Weinshenker BG, Reingold SC, Cohen JA. Diagnosis of Multiple Sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 2018;17:162-73. PMID: 29275977 DOI: 10.1016/S1474-4422(17)30470-2
- Fox RJ, Coffey CS, Conwit R, Cudkowicz ME, Gleason T, Goodman A, Klawiter EC, Matsuda K, McGovern M, Naismith RT, Ashokkumar A, Barnes J, Ecklund D, Klingner E, Koepp M, Long JD, Natarajan S, Thornell B, Yankey J, Bermel RA, Debbins JP, Huang X, Jagodnik P, Lowe MJ, Nakamura K, Narayanan S, Sakaie KE, Thoomukuntla B, Zhou X, Krieger S, Alvarez E, Apperson M, Bashir K, Cohen BA, Coyle PK, Delgado S, Dewitt LD, Flores A, Giesser BS, Goldman MD, Jubelt B, Lava N, Lynch SG, Moses H, Ontaneda D, Perumal JS, Racke M, Repovic P, Riley CS, Severson C, Shinnar S, Suski V, Weinstock-Guttman B, Yadav V, Zabeti A; NN102/SPRINT-MS Trial Investigators. Phase 2 trial of ibudilast in progressive multiple sclerosis. N Engl J Med 2018;379(9):846-55. PMID: 30157388
- Cohen JA, Comi G, Selmaj KW, Bar-Or A, Arnold DL, Steinman L, Hartung HP, Montalban X, Havrdová EK, Cree BAC, Sheffield JK, Minton N, Raghupathi K, Huang V, Kappos L, for the RADIANCE Trial Investigators. Efficacy and safety of the sphingosine 1-phosphate receptor modulator ozanimod or interferon beta-1a in relapsing multiple sclerosis (RADIANCE): a multicentre, randomised, 24-month, phase 3 trial. Lancet Neurol 2019;18(11):1021-33. PMID: 31492652 DOI: 10.1016/S1474-4422(19)30238-8
- Ontaneda D, Tallantyre E, Kalincik T, Planchon SM, Evangelou N. Early highly effective versus escalation treatment approaches in relapsing multiple sclerosis. Lancet Neurol 2019;18(10):973-80. PMID: 31375366
- Mahajan KR, Nakamura K, Cohen JA, Trapp BD, Ontaneda D. Intrinsic and extrinsic mechanisms of thalamic pathology in multiple sclerosis. Ann Neurol 2020;88:81-92. PMID: 32286701
- Kunchok A, Chen JJ, Saadeh RS, Wingerchuk DM, Weinshenker BG, Flanagan EP, Pittock SJ. Application of 2015 Seronegative neuromyelitis optica spectrum disorder diagnostic criteria for patients With myelin oligodendrocyte glycoprotein IgG-associated disorders. JAMA Neurol 2020;77(12):1572-75. PMID: 32777005
- Kunchok A, Aksamit AJ Jr, Davis JM 3rd, Kantarci OH, Keegan BM, Pittock SJ, Weinshenker BG, McKeon A. Association Between Tumor Necrosis Factor Inhibitor Exposure and Inflammatory Central Nervous System Events. JAMA Neurol 2020;77(8):937-46. PMID: 32421186
- Kunchok A, Chen JJ, McKeon A, Mills JR, Flanagan EP, Pittock SJ. Coexistence of myelin oligodendrocyte glycoprotein and aquaporin-4 antibodies in adult and pediatric patients. JAMA Neurol 2020;77(2):257-9. PMID: 31657826
- Ontaneda D, Raza PC, Mahajan KR, Arnold DL, Dwyer MG, Gauthier SA, Greve DN, Harrison DM, Henry RG, Li DKB, Mainero C, Moore W, Narayanan S, Oh J, Patel R, Pelletier D, Rauscher A, Rooney WD, Sicotte NL, Tam R, Reich DS, Azevedo CJ; North American Imaging in Multiple Sclerosis Cooperative (NAIMS). Deep grey matter injury in multiple sclerosis: a NAIMS consensus statement. Brain 2021;144(7):1974-84. PMID: 33757115
- McGinley MP, Goldschmidt CH, Rae-Grant AD. Diagnosis and treatment of multiple sclerosis: a review. JAMA 2021;325(8):765-79. PMID: 33620411
- McGinley MP, Cohen JA. Sphingosine 1-phosphate receptor modulators in multiple sclerosis and other conditions. Lancet 2021;398(10306):1184-94. PMID: 34175020 DOI: 10.1016/S0140-6736(21)00244-0
- Lublin FD, Häring DA, Ganjgahi H, Ocampo A, Hatami F, Čuklina J, Aarden P, Dahlke F, Arnold DL, Wiendl H, Chitnis T, Nichols TE, Kieseier BC, Bermel RA. How patients with multiple sclerosis acquire disability. Brain 2022;145(9):3147-161. PMID: 35104840
- Solomon AJ, Arrambide G, Brownlee WJ, Flanagan EP, Amato MP, Amezcua L, Banwell BL, Barkhof F, Corboy JR, Correale J, Fujihara K, Graves J, Harnegie MP, Hemmer B, Lechner-Scott J, Marrie RA, Newsome SD, Rocca MA, Royal W III, Waubant EL, Yamout B, Cohen JA. Differential diagnosis of suspected multiple sclerosis: an updated consensus approach. Lancet Neurol 2023;22: 750-68. PMID: 37479377 DOI: 10.1016/S1474-4422(23)00148-5
- Majed M, Valencia Sanchez C, Bennett JL, Fryer J, Mulligan MD, Redenbaugh V, McKeon A, Mills JR, Wingerchuk DM, Lennon VA, Weinshenker B, Chen JJ, Flanagan EP, Pittock SJ, Kunchok A. Alterations in aquaporin-4-IgG serostatus in 986 patients: a laboratory-based longitudinal analysis. Ann Neurol 2023;94(4):727-35. PMID: 37314750
- Chataway J, Williams T, Li V, Marrie RA, Ontaneda D, Fox RJ. Clinical trials for progressive multiple sclerosis: progress, new lessons learned, and remaining challenges. Lancet Neurol 2024;23(3):277-301. PMID: 38365380

Application Process
The application and selection process for the Neuroimmunology Fellowship and Neuroimmunology – Clinical and Research Fellowship occurs by the match administered by SF Match and coordinated by Americas Committee for Treatment and Research in MS (ACTRIMS). Applications are accepted beginning approximately 18 months before the planned start date.
Information about the match can be found at:
https://www.sfmatch.org/specialty/neuroimmunology-&-multiple-sclerosis-fellowship/overview
Interested candidates will be requested to submit:
- Curriculum vitae.
- Personal Statement.
- Three letters of recommendation.
- USMLE/COMLEX Score Reports.
- Currently valid ECFMG certificate (applicable for International Medical Graduates only).
Interviews are arranged by invitation.
Contact
Fellowship Director
Jeffrey A. Cohen, MD
216.445.8110
cohenj@ccf.org
Fellowship Associate Directors
Daniel Ontaneda, MD PhD
216.444.0151
ontaned@ccf.org
Amy Kunchok, MD, PhD
216.445.2751
kunchoa@ccf.org
Fellowship Program Coordinator
Sarah Planchon Pope, PhD
216.636.1232
planchs@ccf.org
Neurologic Institute Education Office
nieducation@ccf.org
Clinical Fellows
Outstanding patient care, education of those who serve and research are the three goals the Department of Neurology strives to achieve. As a part of that overall commitment to education, below are the recognized current neurology fellows who value the importance of providing the highest quality of medical care.
2025-2026 Clinical Fellows

Eva Chava Bernfeld, MD
Medical School: Ben Gurion University of the Negev, Be’er Sheva, Israel
Residency: Case Western Reserve University/University Hospitals Cleveland Medical Center, Rainbow Babies and Children’s Hospital and University of Iowa Hospitals and Clinics — Pediatrics and Pediatric Neurology

Amjad Samara, MD
Medical School: An-Najah National University Faculty of Medicine and Health Science, Nablus, Palestine
Residency: Washington University, St. Louis, MI — Neurology

Jeffrey Lambe, MD
Medical School: Royal College of Physicians of Ireland, Dublin, Ireland
Residency: Cleveland Clinic – Neurology

Saira Afzal, MD
Medical School: King Edwards Medical University, Lahore, Pakistan
Residency: Cleveland Clinic Florida – Neurology

Katherine Havard-Coiro, MD
Medical School: Indiana University School of Medicine, Indianapolis IN
Residency: Cleveland Clinic – Neurology

Kaitlyn Palmer, MD
Medical School: Drexel University College of Medicine, Philadelphia, PA
Residency: Cleveland Clinic – Neurology
Living in Cleveland

Cleveland, a vibrant, mid-sized city located on Lake Erie, features a host of cultural attractions, recreational activities, major sporting events and an exploding culinary scene. Cleveland has the second largest theater district in the U.S., the world famous Cleveland Orchestra, a park system featuring 23,700 acres in 18 reservations, and is the birthplace of rock ’n’ roll, home to the Rock ‘n’ Roll Hall of Fame and Museum. Cleveland Clinic is located near the University Circle area, which is the cultural epicenter of Cleveland. This area features Severance Hall home of the Cleveland Orchestra, the Cleveland Museum of Art, several other museums, and Case Western Reserve University. Downtown Cleveland, home to all major sports venues and an exploding culinary scene, is approximately two miles from Cleveland Clinic’s main campus. There are 1-hour flights from Hopkins International Airport to New York, Chicago, and Toronto. There is skiing locally and in surrounding states. The cost of living in Northeast Ohio is quite reasonable.
Clinical Neuroimmunology & Multiple Sclerosis Fellowship - Las Vegas
The Clinical Neuroimmunology and Multiple Sclerosis Fellowship is designed to prepare academically oriented neurologists and physiatrists for a career in patient care and clinical research in multiple sclerosis. The training program is flexible; the specific curriculum and duration are tailored to the fellow’s background, interests, and career goals.
Potential components of training include:
Patient Care
One aspect of the fellowship is supervised patient care to develop specialized expertise in the diagnosis and management of MS and related neuroimmunological disorders. Fellows participate as a member of a multi-disciplinary team that evaluates and treats a large number of patients. Medical neurology visits cover a wide spectrum of issues, including diagnosis, disease management, management of symptoms and psychosocial issues, and evaluation of patients for potential participation in experimental therapy protocols.
The Lou Ruvo Center for Brain Health is a tertiary care center offering expert consultation to healthcare professionals globally, while providing primary ongoing care for patients in Nevada and neighboring states, focusing on neurodegenerative disorders of dementia, movement disorders and neuroimmunology/multiple sclerosis. The Neuroimmunology and Multiple Sclerosis Program cares for approximately 1800 patients annually. The clinical team is comprised of 2 neuroimmunology and multiple sclerosis fellowship trained neurologists and advanced practice providers, a dedicated MS nursing team, social workers for counseling and support services, physical/occupational/speech therapists who have obtained certified MS specialty training, neuropsychiatry, health psychology and neuropsychology staff, and botulinum toxin specialists for spasticity. External rotations include neuro-ophthalmology, rheumatology and physical medicine and rehabilitation. It is possible to arrange time in other areas, such as neuroradiology, autoimmune neurology, or pediatric neuroimmunology, to gain expertise in other immune-mediated disorders of the nervous system. Our center provides comprehensive care for patients with multiple sclerosis and related disorders in a community-based academic setting.
Resources include a dedicated imaging center with on-site 3T MRI, high-resolution monitors for viewing images obtained on any CCF scanner, and workstations for quantitative image processing. We also have a dedicated optical coherence tomography unit.
Experience in Clinical Trials
The other potential focus of the fellowship is training in clinical research, most often experimental therapeutics. In addition to clinical training, fellows pursuing clinical research training divide their time between participation as a sub-investigator in ongoing trials and conducting independent research. We participate in a large number of multiple sclerosis and neuroimmunology clinical trials. In some trials, fellows serve as an examining physician to develop expertise in a standardized neurologic examination, calculating rating scales such as the Kurtzke EDSS, and performing the MS Functional Composite. In other trials, fellows serve as the treating physician under the direction of the Principal Investigator to become familiar with issues involved in patient management within the constraints of a protocol. Fellows gain experience in trial management and implementation by reviewing the consent form, managing regulatory documents, supervising patient recruitment, planning study visits, and working with data coordinators and study monitors to resolve queries.
The research infrastructure for the MS program includes research nurses, data coordinators, and administrative support personnel. The professional staff members participate in clinical research projects (as Principal Investigator or a co-investigator), providing ample opportunities for the fellow to be involved in scientific investigations.
Clinical Research
All fellows pursue some academic activities. Although research is not an emphasis of the one-year clinical program, fellows typically have the opportunity to prepare at least one manuscript for publication or carry out a focused research project. They may also participate as a sub-investigator in a few clinical trials to gain some exposure to clinical trial conduct. There are also opportunities to collaborate with Main Campus in Cleveland on research projects.
Training in Imaging Related to MS
Training in MRI is obtained through reading studies as part routine patient care and the twice-monthly Mellen MRI conference (managed by the fellows) in which studies are reviewed with neuroradiology experts. Fellows also are trained to perform and interpret OCT. Research projects utilizing MRI or OCT are possible.
The one-year clinical fellowship focuses on clinical training, and fellows typically spend most of their time seeing patients.
Application Process
Cleveland Clinic Nevada’s Clinical Neuroimmunology and Multiple Sclerosis Fellowship will be using the SF Match system. One position per year is available with an anticipated start date of July 1st.
The following materials will be requested of you by The Match’s Central Application System (CAS):
- CAS Distribution List (Online Submission).
- Completed CAS application form (Online Submission).
- USMLE Scores or equivalent score reports.
- ECFMG Certificate (applicable to International Graduates).
- Three (3) letters of reference.
- Curriculum Vitae (CV).
Application Timeline
- SF Match Application Starts – Monday, November 3, 2025
- CAS Target Date – Wednesday, February 4, 2026
- Rank List Deadline – Wednesday, April 29, 2026
- Match Results – Wednesday, May 6, 2026
- Anticipated Start Date – Wednesday, July 1, 2027
This is a time of rapid advances in the understanding of the MS disease process, leading to the emergence of an increasing number of treatment options. Numerous institutions are seeking candidates with this type of training.
We look forward to hearing from you.
Living in Las Vegas
While many Las Vegas newcomers are awed by the nightlife and world of entertainment options, they are even more delighted with the myriad of housing options available citywide. Whether you are looking for rural seclusion, a lush, private master-planned community or high-rise living on the Las Vegas Strip, you will find the options endless.
Clark County contains Las Vegas, Henderson and North Las Vegas the three biggest cities in Southern Nevada. Clark County's population based on the most recent U.S. Census figures indicates we have reached nearly two million residents. Las Vegas is known as the entertainment capital of the world and over the last couple of decades has garnered accolades for its fast-growing population, entrepreneurial atmosphere, unlimited housing and vast employment options. Las Vegas continues to expand its non-gaming industry base and is becoming a notable education and research community. Henderson has been consistently measured as one of the fastest growing communities in the nation. Las Vegas' little sister, Henderson has a population of just over 250,000.
Just south of Las Vegas, Henderson is a vibrant suburb. Created for Basic Magnesium, Inc. defense plants during World War II, Henderson continues to evolve with the addition of its own entertainment and recreation. Henderson's main attraction is Lake Mead, the world's largest man-made lake and home to Hoover Dam.
North Las Vegas is the third fastest-growing city in the nation with a population exceeding 200,000, and it is vibrant and independent city. A proactive city government has led the way in creating a technology hub in the area. The city is home to the bulk of Southern Nevada's manufacturing facilities.
Located in the southeastern part of the valley, 25 miles from downtown Las Vegas and 10 miles outside of Henderson lies Boulder City, home of the Hoover Dam and Lake Mead National Recreation Area. This small community preserves the charm of "small" town U.S.A. just minutes from the one of the most exciting cities in the world. Controlled growth and thoughtful planning make Boulder City an ideal choice for those seeking a hometown free from gaming.
Planned Communities you might choose the mountain communities located in west and southwest Las Vegas. Mountain's Edge, Summerlin and Centennial Hills are all neighborhood communities that offer amazing vistas and landscapes. Southern Highlands in southwest Las Vegas is one of the newest areas near the airport and the trendy "south" Strip. You might prefer more established communities in the heart of the city near the Strip and resort corridor in Paradise Valley. There are also beautiful communities in Henderson just south of Las Vegas featuring championship golf courses and country clubs such as Green Valley Ranch, MacDonald's Highlands and Seven Hills.