Atrial fibrillation (AFib) is an irregular heart rhythm that begins in your heart’s upper chambers (atria). Symptoms include fatigue, heart palpitations, trouble breathing and dizziness. Risk factors include high blood pressure, coronary artery disease and having obesity. Medications and procedures (like ablation) can lower your risk of a stroke.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
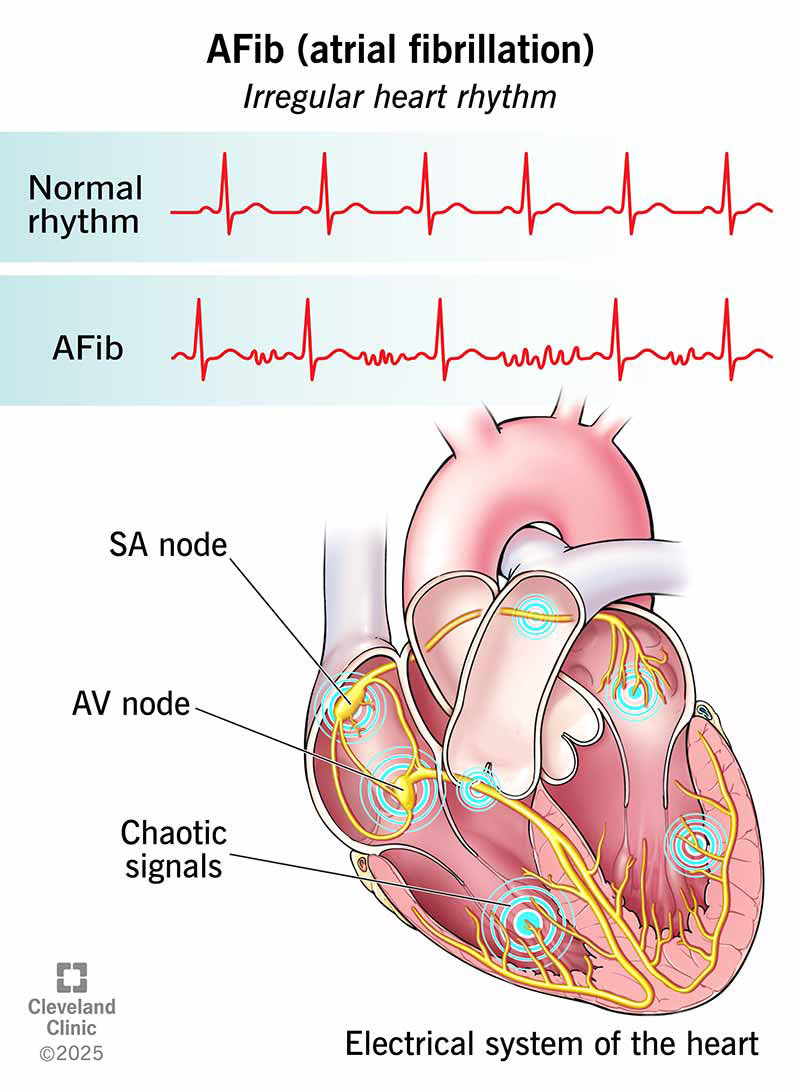
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16765-afib-illustration)
AFib (atrial fibrillation) is an irregular heart rhythm that begins in the upper chambers of your heart. With AFib, your heart’s electrical system doesn’t work as it should. Instead of sending electrical signals in a steady pattern, it sends many different signals at the same time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This causes a fast, chaotic rhythm in your upper chambers (atria). As a result, your atria can’t do a good job of contracting or pumping blood into your lower chambers (ventricles). Your ventricles, which respond to your atria, also contract irregularly, causing a fast, irregular heartbeat. The heartbeat that you feel comes from your ventricles’ contractions.
You can think of Afib like several conductors directing an orchestra instead of just one. The musicians wouldn’t know who to follow or what to do. The music would lose its rhythm.
Atrial fibrillation can lead to serious complications like a stroke or heart failure. That’s why it’s important to learn the symptoms and talk with your healthcare provider about your personal risk factors.
AFib symptoms include:
Whether or not you feel symptoms, being in AFib is serious. It means your heart is out of rhythm. When your heart isn’t beating normally, you have a higher risk of dangerous blood clots forming in your heart and traveling to vital organs such as your brain, resulting in a stroke, as well as other complications. If you have symptoms of AFib, contact your healthcare provider right away.
Advertisement
Call 911 or your local emergency number if you:
Changes to your heart’s tissue and electrical system cause atrial fibrillation. Here’s what can cause such changes:
Having any of the medical conditions listed above raises your risk for AFib. Other risk factors include:
An electrocardiogram (ECG/EKG) diagnoses atrial fibrillation. This test creates a graph of the electrical signals traveling through your heart. The results can show if you have AFib or other types of arrhythmias.
Your provider will also:
AFib is a progressive condition. That means it develops in stages and can get worse over time. Here are the updated stages that healthcare providers use when diagnosing and treating AFib:
You have certain risk factors for AFib, including:
You have changes to your heart’s electrical activity or structure that further raise your risk for AFib. Signs providers look for include:
Advertisement
You’re also at stage 2 if you have certain conditions linked with a high risk for AFib. These include:
An ECG/EKG shows you have atrial fibrillation. But this can mean a lot of different things. You might have symptoms that come and go on their own. Or you might have AFib episodes that persist despite treatment. Symptoms might go away after treatment, but return down the road.
That’s why healthcare providers divide this stage into four substages.
Once you’re diagnosed with AFib, you might transition among any of these substages. For example, persistent AFib might return some time after a successful ablation.
Advertisement
This means you’re no longer trying to manage AFib with treatments and you’re constantly in AFib. You and your healthcare provider make this decision together based on your situation.
Atrial fibrillation treatment involves one or more of the following:
These are things you can do from day to day to help keep AFib from progressing. Lifestyle changes are important across all the stages of AFib — including before you have any symptoms. Your provider will help you:
Your provider may prescribe medications to control your heart rate and/or heart rhythm. These medications can prevent damage to your heart and help reduce symptoms that make you feel uncomfortable or anxious. Your provider may also prescribe medications that lower your risk of blood clots that could lead to a stroke.
The medications you need to manage AFib may change over time. In general, you’ll need to take blood thinners (anticoagulants) if you’re at risk of having a stroke. Providers typically prescribe oral anticoagulants (DOACs) like:
Advertisement
In some cases, providers prescribe warfarin instead of a DOAC.
Medications to manage your heart rate include:
Medications that help your heart beat in a normal (sinus) rhythm include:
Ablation for AFib is an umbrella term for a group of procedures that create scar tissue in your heart. We often think of scars as harmful, but in this case, the scar tissue helps your heart’s electrical system work better. The scars block the abnormal electrical signals to help your heart beat in a normal rhythm.
Specific procedures your cardiologist might recommend for AFib include:
Other procedures that treat AFib include:
Yes. Sometimes, your heart will go back to a normal rhythm on its own. This is the case with paroxysmal AFib. If you have persistent or long-standing AFib, you need treatment to end an episode.
But it’s important to know there’s no cure for AFib. Once you have it, you have it for life. Your provider will help you manage the condition. Treatment can lower your risk of a stroke and help you experience fewer symptoms.
A study published in 2024 found that people with AFib had a shorter life expectancy than those without AFib. The number of years lost from their life expectancy varied by their age at diagnosis. The younger you are at diagnosis, the shorter your life expectancy, and the more years you lose compared to others your age without AFib.
| Age at diagnosis | Average life expectancy |
|---|---|
| 30 years old | 72 years (about 11.3 years shorter than expected) |
| 50 years old | 75 years (about 9.2 years shorter than expected) |
| 70 years old | 82 years (about 5.4 years shorter than expected) |
| Age at diagnosis | |
| 30 years old | |
| Average life expectancy | |
| 72 years (about 11.3 years shorter than expected) | |
| 50 years old | |
| Average life expectancy | |
| 75 years (about 9.2 years shorter than expected) | |
| 70 years old | |
| Average life expectancy | |
| 82 years (about 5.4 years shorter than expected) |
Remember that statistics just tell part of the story. Working closely with your healthcare team to manage AFib and any other medical conditions can give you the best chance at a long life.
The same habits that lower your risk of Afib help you feel better when you have it. Eating nutritious foods and getting 30 minutes of physical activity five days a week helps your heart. You can break up your activity into 10-minute chunks to make it easier. Cutting out tobacco products and alcohol is good for your heart, too.
There’s no single schedule to follow. It all depends on your symptoms and treatment plan, and whether you need follow-ups after a procedure. So, it’s important to talk with your provider and make a plan together. Make sure you go to all your scheduled appointments. Keep track of the medications you’re taking and bring a list of your medications to every visit. It’s also a good idea to keep the list in your wallet so it’s with you in emergencies.
At each visit, be sure to share any new symptoms or problems you’re having, like side effects from medication. Be sure to ask your provider before taking over-the-counter (OTC) medicines, like those for cold and flu, and nutritional supplements. Sometimes, these products can affect your heart rate or interact with your prescription medications.
Questions to consider asking your provider may include:
If you think you have Afib symptoms, it’s important to call your healthcare provider right away to discuss how you’re feeling. Your provider may ask you to check your pulse. If it feels erratic or weak, that could be a sign you’re in Afib.
But sometimes, you might not notice any changes in your pulse, especially if your Afib isn’t advanced. You may instead just feel tired or out of breath. You may not know if your symptoms are from Afib or something else. That’s why a call to your provider is essential. You can’t diagnose Afib yourself.
More than 33 million people age 55+ worldwide have an Afib diagnosis. Estimates predict that 12 million people in the U.S. will have Afib by 2030. Afib causes nearly half a million hospitalizations a year in the U.S. and leads to more and more deaths with each passing year.
An AFib diagnosis can feel scary, confusing or overwhelming. But you’re not alone. You’re one of the millions of people learning new strategies for managing AFib while still enjoying life. Your healthcare provider can tell you more about treatment options, resources and support communities.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
