Left atrial appendage (LAA) closure is a procedure that blocks or closes the opening to your LAA to keep blood clots from leaving there and going into your bloodstream. This prevents strokes in people with atrial fibrillation, but without blood thinners. This appendage in one of your heart’s upper chambers doesn’t have a function.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
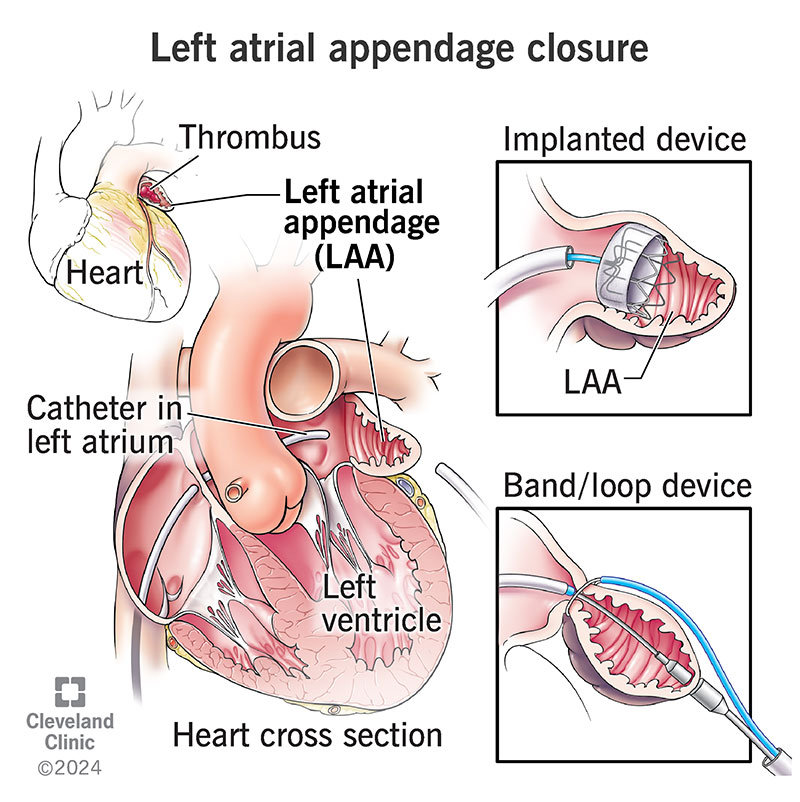
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17167-left-atrial-appendage-closure)
Left atrial appendage closure is a surgical or minimally invasive procedure to seal off your left atrial appendage (LAA). This is a small sac in the muscle wall of your left atrium (top left chamber of your heart). Removing it or closing it off can reduce your risk of stroke and end the need to take blood thinners.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Among people with atrial fibrillation (Afib) who don’t have valve disease, most of the blood clots that happen in the left atrium start in the LAA.
Normal hearts contract with each heartbeat, squeezing the blood in your left atrium and LAA out into your left ventricle (bottom left chamber of the heart). When you have Afib, the electrical impulses that control your heartbeat don’t travel in an orderly way. They can be fast and chaotic, which doesn’t give your atria time to squeeze blood into your ventricles.
Because the LAA is a pouch, blood collects there and can form clots. When your heart pumps out blood clots, they can cause a stroke. People with Afib are three to five times more likely to have a stroke than the general population. While this is unsettling, your provider can help you protect yourself with a solution that works for you. This can involve medications that make it more difficult for these blood clots to form or closing off the left atrial appendage.
Your heart can keep doing its job with a closed left atrial appendage.
Thousands of people worldwide have had an LAA closure. Providers use different methods and devices, like:
Advertisement
LAA closure reduces the stroke risk associated with Afib. But it doesn’t treat the Afib itself. Left atrial appendage closure can benefit people who have an increased risk of stroke due to Afib. If you’re at risk of getting blood clots in your left atrium/left atrial appendage, your healthcare provider may recommend sealing off your LAA to reduce your risk of stroke from Afib. They can do this instead of prescribing a blood thinner like warfarin (Coumadin® or Jantoven®), apixaban (Eliquis®), rivaroxaban (Xarelto®) or dabigatran (Pradaxa®).
Many people have concerns about, or dislike, taking warfarin. Some of the reasons for this are:
People with Afib who don’t have heart valve disease can take other medications — apixaban, dabigatran and rivaroxaban. But some people have concerns and problems with these medications:
Before an LAA closure, you’ll get a transesophageal echocardiogram (TEE) and/or cardiac CT. This gives your provider dimensions of your left atrial appendage. This matters because left atrial appendages vary from person to person. Researchers have compared the left atrial appendage’s shape to a chicken wing, cactus, windsock or cauliflower.
Your provider may also do three-dimensional printing to help choose the correct device and the right size.
You’ll need to fast (stop eating and drinking) at a certain time before your procedure. Your provider will tell you when to fast.
You’ll receive anesthesia of some type, depending on which procedure you’re having.
If you’re having heart surgery for other reasons, like coronary artery disease or valve disease, your healthcare provider frequently can remove your left atrial appendage at the same time. They may sew or staple the area closed. This is a surgical left atrial appendage closure.
In a minimally invasive approach, they can use a catheter to insert a special device to close or block your left atrial appendage. These devices may act as a plug in your left atrial appendage’s opening to your left atrium. Other devices tie or clamp your left atrial appendage closed.
Advertisement
For a device your provider uses a catheter to implant, they will:
Several types of imaging guide your provider while they work inside your heart. Types of imaging they use include:
After your surgery or minimally invasive procedure, you may:
People who get an LAA closure can:
Left atrial appendage closure complications may include:
Advertisement
If you had your LAA closure as part of a heart surgery for another issue, your recovery time will vary depending on which other surgery you had.
If you had a minimally invasive procedure using a catheter to put in a left atrial appendage closure device, your recovery will be quicker. You may be able to go home the next day.
After getting a device, you’ll need to take an anticoagulant (blood thinner) and aspirin for 45 days. This is how long it takes your body’s tissue to form around the device so there aren’t any gaps around it. Then, you’ll stop taking an anticoagulant and switch to clopidogrel (Plavix®) and aspirin for six months.
You may be on aspirin for the long term.
You’ll have another transesophageal echo (TEE) at a follow-up visit 45 days after your procedure. This helps your provider see if your left atrial appendage is fully blocked.
If the TEE shows that your left atrial appendage isn’t blocked, you’ll keep taking the anticoagulant and have another TEE and follow-up visit after six months.
Once your left atrial appendage is blocked, you’ll have an annual follow-up visit with your provider.
Advertisement
Researchers have linked LAA closure with suture to a 40% decrease in the risk of a blood clot, and over 90% with clip or surgical excision. They found an 80% decrease in strokes in device studies. Some devices have rates above 95% for successful placement.
While there’s no surefire way to prevent strokes, removing or blocking your left atrial appendage reduces your risk significantly. This is because 90% of strokes that start in an upper heart chamber start in your LAA.
In addition to going to your scheduled visits, you should contact your provider if you have:
It can be hard living with the threat of stroke from Afib, especially if you have trouble with blood thinners. Deciding on a left atrial appendage closure is a personal decision. After talking with your healthcare provider and discussing your options, you can make an informed decision. The procedure isn’t right for everyone. But if you have Afib, it’s an option you can consider. Be sure to ask your provider any questions you have about the procedure.
If you have a left atrial appendage closure procedure, keep taking your medicines until your provider tells you to stop. Follow-up visits are important, too. These ensure you’re healing and your device is fitting well.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
