If you have diabetes, you’re at increased risk of foot conditions and complications, like open sores and infections. Because of this, it’s important to do everything you can to take care of your feet and manage diabetes well. If you develop foot issues, see your healthcare provider as soon as possible. Early treatment is key to preventing serious complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
People with diabetes are at an increased risk of foot conditions and complications if they have diabetes-related neuropathy and/or poor circulation. Diabetes-related neuropathy happens when you experience nerve damage due to persistently high blood sugar (hyperglycemia). It most commonly affects your feet.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Diabetes-related foot complications can happen due to a snowball effect of issues:
For all these reasons, taking care of your feet and managing diabetes well are very important. Several simple steps can help you prevent foot issues.
Any skin-, nerve- or circulation-related issue with your foot has an increased risk of turning into an infection or another complication when you have diabetes. Examples of foot and toe conditions that could lead to complications include:
Advertisement
Foot and toe ulcers (open sores) are some of the most common types of foot problems for people with diabetes. About 15% of people with diabetes will get a foot or toe ulcer. The ulcers typically develop in areas where your foot repeatedly rubs or presses against shoes or other surfaces.
Ulcers can lead to infections. Sometimes, the infection doesn’t go away, and you may need to have part of your foot or toe surgically removed (amputated). Know that early treatment greatly reduces your risk of amputation.
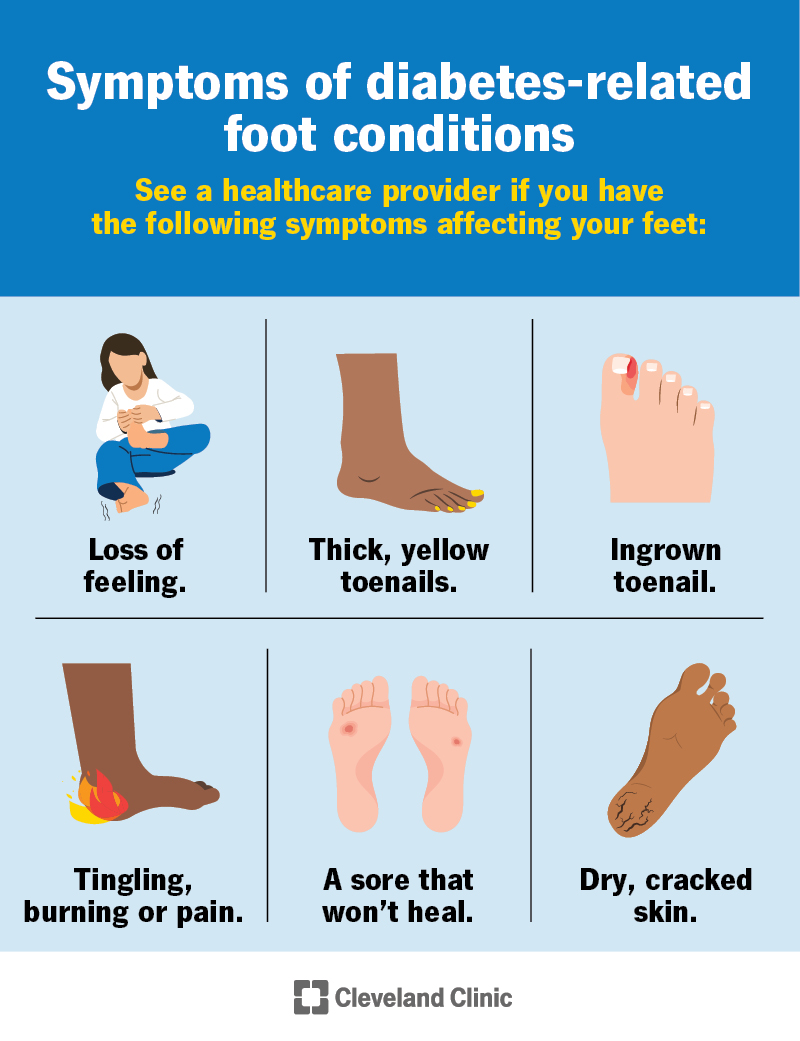
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21510-diabetic-feet)
Symptoms of diabetes-related foot conditions vary based on the type. But in general, you should look out for the following symptoms:
See your healthcare provider if you have these symptoms.
Gangrene and Charcot foot are the main serious complications of diabetes-related foot conditions.
A foot infection that’s not treated in time can lead to gangrene. Gangrene is a medical emergency in which blood stops flowing to a specific part of your body, and tissues in that area die. Without prompt treatment, gangrene can be fatal.
Symptoms of gangrene include:
Go to the emergency room (ER) if you have signs of gangrene.
Charcot foot is a rare complication of diabetes-related neuropathy. If it’s not treated soon enough, Charcot foot can make the joints in your foot collapse and permanently affect your ability to use your foot. It can also make it more likely for an infection in your foot to worsen or spread to the rest of your body.
Early symptoms of Charcot foot include:
See your healthcare provider if you have these early signs.
The two main underlying causes of diabetes-related foot conditions are:
Advertisement
Perpetually high blood sugar levels can damage nerves and small blood vessels. Each person is different, so it’s impossible to predict how high blood sugar levels have to be — and for how long — to cause neuropathy or PAD. One study on people with Type 2 diabetes shows that having an A1C over 7% for at least 3 years increases your risk of diabetes-related neuropathy.
Poor foot care, like wearing ill-fitting shoes, walking barefoot or not treating sores and cuts with basic first-aid methods, can also increase your risk of foot conditions.
To diagnose diabetes-related foot conditions, a healthcare provider will:
If you have a diabetes-related ulcer or blister, your provider will likely:
Treatment for diabetes-related foot conditions depends on the type. It’s essential to get medical help for diabetes-related foot conditions — don’t try to treat them yourself. Treatment for these issues may involve a podiatrist — a healthcare provider who specializes in foot care.
Advertisement
If you have a diabetes-related ulcer, for example, your provider may:
Depending on how severe the infection is, your provider may recommend hospitalization. Sometimes, amputation is necessary to prevent infection from spreading to other parts of your body. Early treatment greatly reduces your risk of amputation.
Diabetes-related foot conditions are fairly common in people who’ve had diabetes for a long time. Even with foot checks and careful blood glucose monitoring, some people with diabetes develop infections.
Your outlook depends on factors, like:
Your healthcare provider will give you a better idea of what to expect based on your unique situation.
There are several steps you can take to help prevent diabetes-related foot conditions.
Advertisement
The most important step is to manage your blood sugar and diabetes well to try to avoid or delay diabetes-related neuropathy and blood flow issues. See your diabetes healthcare provider (like an endocrinologist) regularly for help with your management plan. Your medication needs will change as your life changes. Also, ask about advances in diabetes management technology, like continuous glucose monitoring (CGM), that can help you.
You can also reduce the risk of diabetes-related foot problems by:
It’s just as important to avoid certain things. Don’t:
Visit your healthcare provider or foot specialist (podiatrist) if you have any of these symptoms affecting your feet or toes:
It’s never too early to ask your healthcare provider about how to care for your feet if you have diabetes. Some questions that may be helpful to ask include:
There’s a lot to manage when you have diabetes — from monitoring your glucose levels and taking medications to carefully planning meals and going to medical appointments. Your feet might be an afterthought. But adding your feet to your diabetes care checklist is important. There are several steps you can take to prevent foot issues and complications. If you have questions or concerns about the health of your feet, don’t hesitate to reach out to your healthcare provider. They’re available to help you put your best foot forward.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you’ve been living with diabetes for years or you’re newly diagnosed, you want experts you can trust. Our team at Cleveland Clinic is here to help.
