Strokes happen when a blood clot or broken vessel prevents blood from getting to your brain. They can be fatal and need immediate treatment. Call 911 or your local emergency services number right away if you think you or someone you’re with is having a stroke. The BE FAST acronym can help you spot symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_8nebjroh/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
A stroke is a medical emergency. Learn what to do if you or a loved one is having a stroke.
A stroke is a medical emergency that happens when something prevents your brain from getting enough blood flow. A blocked blood vessel or bleeding in your brain can cause strokes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Healthcare providers sometimes refer to strokes as cerebrovascular accidents (CVAs) or brain attacks.
Strokes are the second leading cause of death worldwide and the fifth most common in the U.S.
If you think you or someone you’re with is having a stroke, immediately call 911 or your local emergency services number. Strokes are life-threatening and can be fatal. The sooner someone is diagnosed and treated, the more likely it is they’ll survive a stroke. Every second counts.
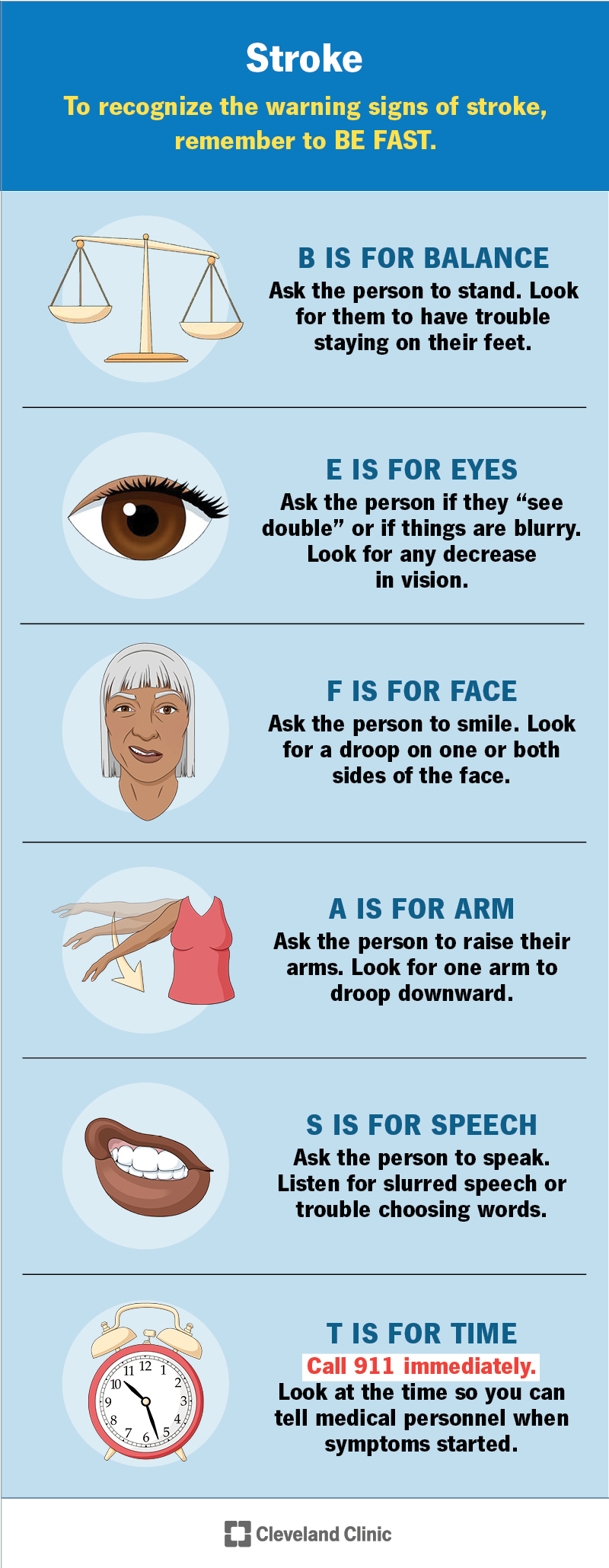
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/5601-stroke)
A stroke can cause different symptoms depending on which area of your brain it affects. Some of the most common symptoms include:
Advertisement
A stroke lasts as long as your brain isn’t getting the right amount of blood flow. Your brain cells die if they go too long without oxygen from fresh blood. If enough brain cells in an area die, the damage becomes permanent. This can cause permanent disabilities and other changes in how you can use your body.
Restoring your normal blood flow may prevent that permanent damage or reduce its severity. That’s why time is critical in treating a stroke.
Even after you receive treatment, it’s common for the effects to linger. Symptoms and after-effects can continue for a year or longer.
Strokes can cause lots of different symptoms. To recognize the warning signs of a stroke in yourself or a loved one, remember the acronym BE FAST:
There are two types of strokes.
Ischemic strokes usually happen because a blood clot blocks a blood vessel connected to your brain. Issues that can cause these kinds of clots include:
Hemorrhagic strokes happen when a blood vessel in your brain breaks or tears (ruptures). Causes can include:
A transient ischemic attack (TIA) — sometimes called a “mini-stroke” — is like a stroke, but the effects are temporary. These are often warning signs that a person has a very high risk of having a true stroke soon. A person who has a TIA needs emergency medical care as soon as possible.
Anybody can have a stroke, but some groups have a higher risk, including people who:
Advertisement
Having certain health conditions can increase your stroke risk, including:
A healthcare provider will diagnose a stroke using a combination of a neurological exam and tests. Providers in the emergency room may diagnose a stroke if emergency services transport you to the ER.
Your provider will use some of the following tests to confirm that you’ve had a stroke:
The treatments you’ll need will depend on a few factors, including:
Your providers will restore normal blood flow to your brain as fast as possible to limit the risk of permanent brain damage.
If you experience an ischemic stroke, your providers will break up or remove the blood clot that caused it. You’ll need thrombolytic medications and/or surgery (usually a mechanical thrombectomy). Your providers may also give you medications to manage your blood pressure.
If you have a hemorrhagic stroke, your providers will control the bleeding that caused it. You’ll need medications to stop the bleeding in your brain and manage your blood pressure. You may need surgery to reduce the increased intracranial pressure around your brain.
Advertisement
Your healthcare providers or surgeon will tell you exactly which treatments are best for you, what to expect and how long it will take to recover.
Stroke rehab is an important part of stroke treatment. You’ll need rehab to help you adjust to changes in your brain and body after a stroke. You may need to regain abilities you had before or adjust to new or different disabilities. You might need a combination of:
It’s hard for experts to estimate a stroke survival rate that applies to everyone. Strokes can be fatal, and they can cause permanent disabilities. But there’s no one set recovery timeline or outlook that’s accurate for everyone.
Ischemic strokes usually have better outcomes than hemorrhagic strokes, but that doesn’t mean your recovery will be easier, faster or better if you have one type or the other.
Advertisement
Everyone’s body responds differently to a stroke. What you can expect (the prognosis) after a stroke depends on a few factors, including:
Most people take a few months to recover after a stroke. Your provider will tell you what to expect. They’ll help you set recovery goals and expectations that fit your unique health and situation.
Maintaining your overall health is the best way to reduce your stroke risk. Try to:
Visit a healthcare provider for a check-up every year (or as often as they suggest). Many of the health conditions and issues that can cause stroke develop and build up over time, and may not cause symptoms you can notice. Many people with high blood pressure never feel or sense anything wrong. Your provider will help you catch and manage any warning signs before they increase your risk of a stroke later on.
Recovering and rehabbing after a stroke is hard work. Once you and your provider finalize your treatment plan, follow it as closely as possible. In general, you should:
Call 911 (or your local emergency services number) if you think you’re experiencing stroke symptoms again. Another stroke has an even higher risk of causing severe complications and being fatal. Don’t wait to call for help or go to the emergency room.
People who’ve had a stroke have an increased risk of other potentially serious complications, including:
Call emergency services or go to the ER if you think you’re experiencing any symptoms of these complications.
You might want to ask your provider a few questions, including:
You know your body better than anyone, and you know when something is off or doesn’t feel right. A stroke is a medical emergency. Call for help right away if you think you’re having a stroke. Getting diagnosed and treated as soon as possible is the best way to increase your chances of survival and recovery.
Having a stroke can be a sudden, life-changing event. Recovery is hard work, but it’s worth it. Don’t forget to stop and appreciate how far you’ve come. Celebrate your successes — every milestone is a big accomplishment during your recovery.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
After a stroke, it’s essential to get treated right away. Cleveland Clinic’s stroke care specialists can help you manage recovery and improve your quality of life.
