Low testosterone (male hypogonadism) is a condition in which your testicles don’t produce enough testosterone. It has several possible causes, including conditions or injuries affecting your testicles, pituitary gland or hypothalamus. It’s treatable with testosterone replacement therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
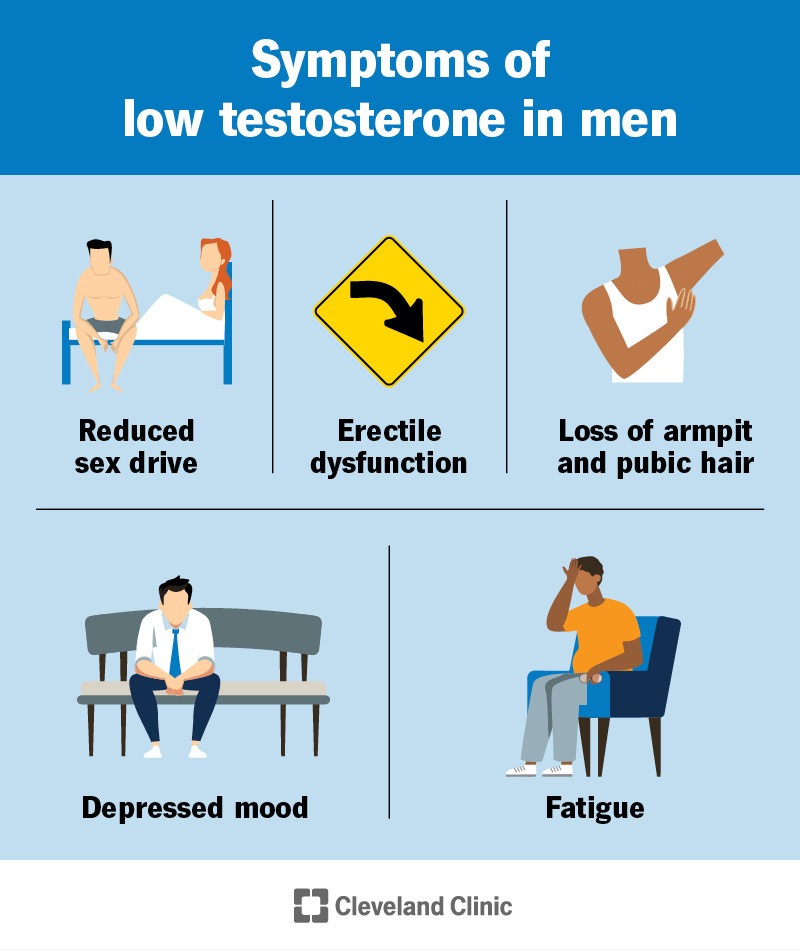
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15603-low-testosterone-male-hypogonadism)
Low testosterone (male hypogonadism) is a condition in which your testicles don’t produce enough testosterone (the male sex hormone). More specifically, the Leydig cells in your testicles make testosterone.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Low testosterone causes different symptoms at different ages. Testosterone levels in adults naturally decline with age.
Other names for low testosterone and male hypogonadism include:
Testosterone is the main androgen. It stimulates the development of male characteristics and is essential for sperm production (spermatogenesis). Levels of testosterone are naturally much higher in men than women.
In men, testosterone helps maintain and develop:
Your body usually tightly controls the levels of testosterone in your blood. Levels are typically highest in the morning and decline through the day.
Your hypothalamus and pituitary gland normally control the amount of testosterone your testicles produce and release.
Your hypothalamus releases gonadotropin-releasing hormone (GnRH), which triggers your pituitary gland to release luteinizing hormone (LH). LH then travels to your gonads (testicles or ovaries) and stimulates the production and release of testosterone. Your pituitary also releases follicle-stimulating hormone (FSH) to cause sperm production.
Advertisement
Any issue with your testicles, hypothalamus or pituitary gland can cause low testosterone (male hypogonadism).
The American Urology Association (AUA) considers low blood testosterone to be less than 300 nanograms per deciliter (ng/dL) for adults.
However, some researchers and healthcare providers disagree with this and feel that levels below 250 ng/dL are low. Providers also take symptoms into consideration when diagnosing low testosterone.
Male hypogonadism is a medical condition that can affect people with testicles at any age from birth through adulthood.
Low testosterone is more likely to affect people who:
It’s difficult for researchers to estimate how common low testosterone is since different studies have different definitions for low testosterone.
Data suggest that about 2% of men may have low testosterone. And other studies have estimated that more than 8% of men aged 50 to 79 years have low testosterone.
Symptoms of low testosterone can vary considerably, particularly by age.
Symptoms that highly suggest low testosterone in men include:
Other symptoms of low testosterone in men include:
Low testosterone before or during puberty for boys:
There are several possible causes of low testosterone. The two types of male hypogonadism are:
Causes of primary and secondary hypogonadism are also divided into either congenital (at birth) or acquired (developed later in childhood or adulthood).
Primary hypogonadism happens when something is wrong with your testicles that doesn’t allow them to make normal levels of testosterone.
Another name for primary hypogonadism is hypergonadotropic hypogonadism. In this type, your pituitary gland produces more luteinizing hormone (LH) and follicle-stimulating hormone (FSH) (known as gonadotropins) in response to low testosterone levels. The high levels of these hormones would normally tell your testicles to produce more testosterone and sperm. However, if you have damaged (most commonly related to prior chemotherapy) or missing testicles, they can’t respond to the increased levels of gonadotropins. As a result, your testicles make too little or no testosterone and sperm.
Advertisement
Sometimes in primary hypogonadism testosterone levels are within the normal range and gonadotropins are high. Your specialist will help you understand if you need treatment, even with normal testosterone levels.
Congenital conditions that affect your testicles and can lead to primary hypogonadism include:
Acquired conditions that affect your testicles and can lead to primary hypogonadism include:
Advertisement
Conditions that affect how your hypothalamus and/or pituitary gland cause secondary hypogonadism. This is known as hypogonadotropic hypogonadism because there are low levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Those low levels cause decreased testosterone and sperm production.
Congenital conditions that can lead to secondary hypogonadism include:
Acquired conditions that can lead to secondary hypogonadism include:
Advertisement
Late-onset hypogonadism (LOH) is a type of secondary male hypogonadism that results from normal aging. As males age they have a deterioration of hypothalamic-pituitary function and Leydig cell function that decrease testosterone and/or sperm production.
LOH and low testosterone are more common in men who have Type 2 diabetes, overweight and/or obesity.
In one study, 30% of men who were overweight had low testosterone, compared to only 6% of those with weight in the normal range. In another study, 25% of men with Type 2 diabetes had low testosterone, compared to 13% of those without diabetes.
If you have signs and symptoms of low testosterone, a healthcare provider will perform a physical exam. They’ll also ask questions about your medical history, medications you take or have taken, smoking history and any symptoms you currently have. Blood tests may be ordered.
To make a diagnosis, a provider will consider your specific signs, symptoms and any blood test results.
The following tests can help confirm low testosterone and determine the cause:
Healthcare providers treat low testosterone (male hypogonadism) with testosterone replacement therapy. Testosterone replacement therapy has several different forms, including:
You may not be able to receive testosterone replacement therapy if you have a history of the following:
The side effects of testosterone replacement therapy include:
Laboratory abnormalities that can occur with testosterone replacement therapy include:
There’s no one-time fix for low testosterone. However, consistent hormone replacement therapy helps improve sex drive, ease symptoms of depression and increase energy levels for those experiencing low testosterone. Treatment may also boost muscle mass and bone density.
The mortality of men with testosterone deficiency is significantly higher than among men with normal testosterone levels. But, it is unclear whether replacing testosterone to a normal level reduces that increased mortality. Treatment is largely focused on the treatment of symptoms, not the specific testosterone level.
For congenital hypogonadism, testosterone replacement therapy often helps prevent problems related to delayed puberty.
Healthcare providers and medical researchers don’t know how to prevent low testosterone from genetic conditions or damage to your testicles, hypothalamus or pituitary gland.
Lifestyle habits that may help keep testosterone levels normal include:
If you’re taking hormone replacement therapy, regular follow-up appointments with a healthcare provider are important.
If you’re experiencing symptoms of low testosterone, such as a decrease in sex drive and hot flashes, talk to a healthcare provider. They will evaluate you and may order blood tests.
If your child isn’t showing signs of puberty by the age of 14, talk to their pediatrician.
Many people shrug off the symptoms associated with low testosterone as an unpleasant part of getting older. But you should address symptoms that interfere with your quality of life. If you’re noticing bothersome signs of low testosterone, see a provider and discuss your options for treatment.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Have a low sex drive or trouble with erections? Low testosterone might be the cause. Cleveland Clinic’s experts can help balance your hormones.
