Azoospermia means there’s no sperm in your ejaculate. Its causes include a blockage along the reproductive tract, hormonal problems, ejaculation problems or issues with testicular structure or function. Many causes are treatable. For other causes, it may be possible to retrieve live sperm to be used in assisted reproductive techniques like IVF.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
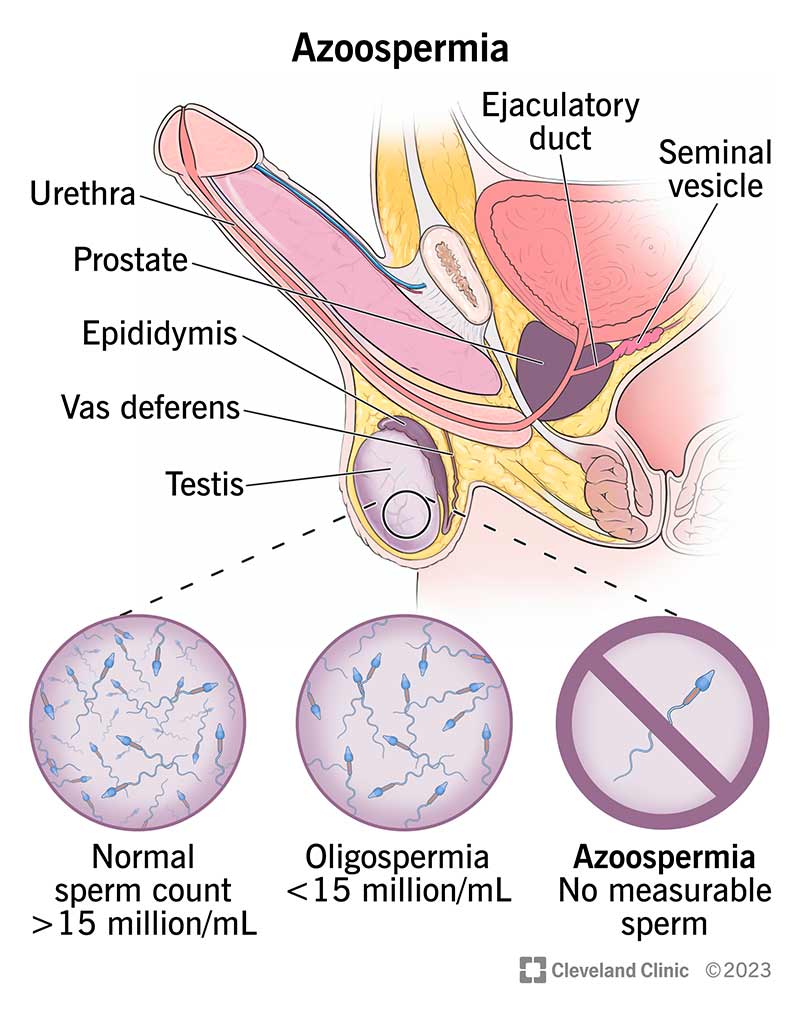
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15441-azoospermia)
Azoospermia is a condition where you have no measurable sperm in your ejaculate (semen).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Typically, testicles produce sperm. Sperm travels through parts of your reproductive system and mixes with fluids to form semen. Semen is the fluid that your penis releases during ejaculation. If you have azoospermia, you may have semen — but there’s no sperm in it. Sometimes, azoospermia is referred to as having “no sperm count.”
Some people are born with no sperm count while some develop it as a teenager or adult. Medication and surgery can help treat azoospermia in certain situations. Just because you have the condition doesn’t mean you can’t have biological children.
There are three types of azoospermia:
Advertisement
Azoospermia affects about 1% of all men.
You usually don’t realize you have the condition until you begin trying to conceive a child with your partner without success. Some people have symptoms related to the underlying cause. For example, you could have low libido due to hormonal imbalance or a lump on your testicles from an infection.
Causes of azoospermia can be an obstruction or blockage (most common), or something else like genetics or hormone imbalances.
Blockages occur most commonly in the epididymis (corkscrew-shaped duct where sperm matures), vas deferens and ejaculatory duct (tube that sperm goes through to mix with fluid and form semen). These obstructions essentially form a roadblock and don’t allow sperm to leave your testicles.
Problems that can cause blockages include:
Nonobstructive causes of azoospermia can include genetics or hormonal disorders. As the name implies, there’s no blockage or obstruction causing there to be no sperm.
Causes of pretesticular and testicular azoospermia include:
Healthcare providers diagnose azoospermia if, on two separate occasions, your semen analysis shows no sperm. A sperm analysis usually comes after a couple is trying to get pregnant without success.
To find the cause of azoospermia, your healthcare provider will take your full medical history, including asking questions about:
Advertisement
Your healthcare provider will also conduct a thorough physical examination, paying close attention to the areas of your scrotum. It may also include a rectal exam.
Treatment of azoospermia depends on the cause. Genetic testing and counseling are often an important part of understanding and treating azoospermia. Treatment approaches include:
If the cause of azoospermia is thought to be something that could be passed on to children, your healthcare provider may recommend genetic counseling.
Advertisement
Yes, it can, but it depends on the type of azoospermia. For example, if a blockage is causing you not to have any sperm, surgery to fix the blockage may result in having sperm in your semen.
There may be a way to cure or reverse azoospermia depending on what causes it. Some causes don’t have a cure.
Every cause of azoospermia has a different prognosis. Many causes of azoospermia can be reversed. You and your healthcare team will work together to determine the cause of your azoospermia and treatment options. Hormonal problems and obstructive causes of azoospermia are usually treatable, and fertility can potentially be restored. If testicular disorders are the cause, it’s still possible to retrieve live sperm to be used in assisted reproductive techniques like IVF.
Yes, you still may be able to get pregnant naturally. This depends on the type of azoospermia your partner has and if it’s treatable. Your healthcare provider is the best person to discuss treatment and family planning with.
It depends on the cause of azoospermia. If the cause is testicular and requires surgical sperm retrieval, then IVF is the only option. If the azoospermia is treatable, couples may be able to avoid IVF.
Advertisement
There’s no known way to prevent the genetic conditions that cause azoospermia. If your azoospermia isn’t a genetic problem, doing the following can help lessen the chance of azoospermia:
Receiving an azoospermia diagnosis can have physical and emotional side effects. It’s important to rely on your healthcare provider’s expertise and lean on your partner while you navigate the best treatment. Your provider may recommend tests to get to the root cause of why you have no sperm. In the meantime, talk to your partner, family or friends about how you’re feeling. It’s normal to feel upset about a setback like this, but don’t let hopelessness set in. Many people go on to have biological children.
Let your healthcare provider know if you and your partner are unsuccessful at getting pregnant after 12 months of regular, unprotected intercourse, or if you have concerns regarding your fertility. This is often the first sign that a condition is affecting sperm production. Getting a sperm test to see how much sperm you have may be one of the first things your healthcare provider recommends.
It’s normal to have questions if you’re told you have no sperm. Questions to ask your healthcare provider could include:
Hearing that something is standing in the way of expanding your family can be disappointing. While you may feel lots of emotions when you hear you don’t have sperm, try to relax until your healthcare provider can get to the root cause of the problem. Having no sperm count doesn’t mean you won’t have children. Your provider may be able to retrieve sperm from your testicles to use for procedures like IVF. Be sure to discuss all your concerns and the possible treatment options with your provider.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Infertility can change your plans. Cleveland Clinic’s experts can work with you to get to the bottom of male infertility and create a customized treatment plan.
