Prader-Willi syndrome is a rare genetic condition that affects a child’s metabolism. It can also affect your child’s body and behavior. This condition causes your child to have a strong appetite and not feel full after meals. Supportive therapies and diet management help treat PWS and prevent complications that can affect your child’s health.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Prader-Willi syndrome (PWS) is a rare genetic condition that affects your child’s metabolism and causes changes to their body and behavior. They have severe low muscle tone and poor feeding during early infancy, followed by a tremendous appetite that develops between 2 and 6 years of age. This can lead to severe obesity if excessive eating isn’t managed.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
PWS typically also causes a delay in childhood milestones and puberty. Although rare, life-threatening complications can occur and include respiratory illnesses, obesity-related cardiovascular problems, sleep apnea and diabetes.
Anyone can develop Prader-Willi syndrome because it’s a genetic condition that happens randomly when reproductive cells form. In rare cases, you can inherit the condition if it runs in your biological family history.
Throughout the world, PWS affects an estimated 1 in 10,000 to 30,000 people.
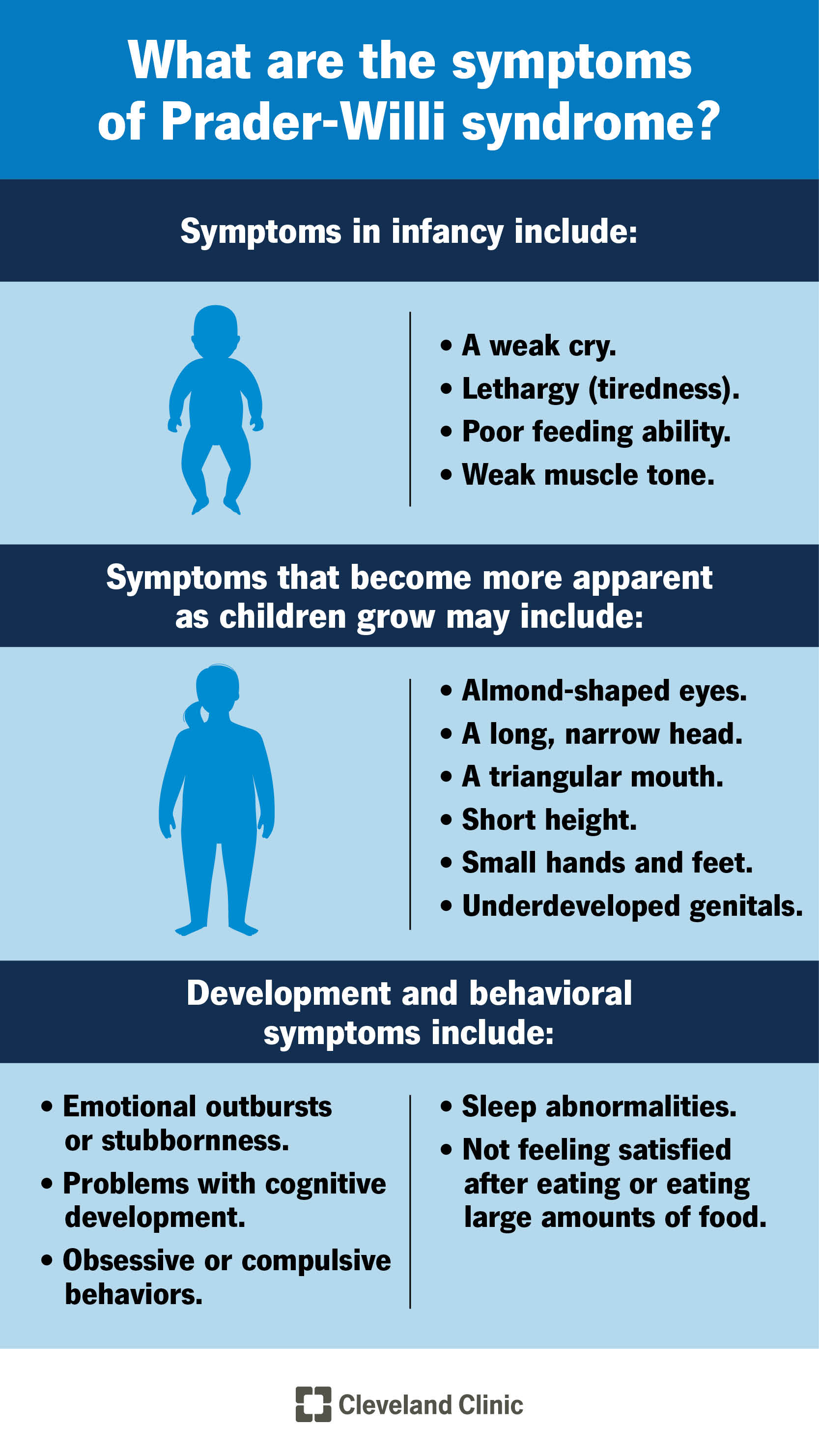
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21016-prader-willi-syndrome)
Prader-Willi syndrome affects each person differently. Symptoms that appear in infancy may include:
Symptoms that affect your child’s body may be present at birth but become more apparent as they grow. These may include:
Additional symptoms that affect your child’s development and behavior include:
Advertisement
Hyperphagia may lead to class III obesity, which increases the likelihood of other complications, such as diabetes and heart disease.
Genes on chromosome 15 that lose function cause Prader-Willi syndrome. At conception, you inherit one copy of chromosome 15 from each of your biological parents. The paternal copy of chromosome 15 is the only one that activates or turns on. The maternal copy is turned off. Both copies are necessary for your genes to get the instructions your body needs to function. This process is called genomic imprinting.
There are different causes of this genetic change to chromosome 15:
Chromosome 15 is responsible for providing instructions for making small nucleolar RNAs (snoRNAs). The job of snoRNAs is to regulate the function of other RNA molecules. RNA molecules create proteins that help cells complete many functions within your body. A change to chromosome 15 limits its ability to create snoRNAs or they don’t receive the instructions they need to complete their jobs correctly.
A healthcare provider will diagnose Prader-Willi syndrome after a physical exam and genetic tests. A provider will look for physical signs of the condition during the exam and ask you questions about your child’s symptoms, including their eating habits and behavior. If your provider suspects PWS, they’ll run a genetic test, which is a blood test that detects abnormalities due to changes to your child’s DNA.
Treatment for Prader-Willi syndrome focuses on managing symptoms and preventing complications. Treatment could include:
Advertisement
Many people with Prader-Willi syndrome develop obesity from overeating. Complications from obesity may include:
Obesity is a complex but manageable condition. Your child’s healthcare provider can offer guidance on how you can help your child and prevent complications.
With early and ongoing treatment, many individuals with Prader-Willi syndrome have a normal lifespan. Needing extra help in school is common. Each person with PWS needs lifelong support to achieve as much independence as possible. Your provider might recommend that you visit a nutritionist to help facilitate a meal plan and diet that can help your child manage their eating. Meeting with a mental health professional or joining a support group is a great resource for parents and families. It can help them find ways to adapt and learn how to help their child grow and meet their full potential.
There isn’t a cure for Prader-Willi syndrome. Research is ongoing to learn more about the condition.
You can’t prevent Prader-Willi syndrome because it’s a genetic condition. Many cases are the result of a random genetic change that’s unpredictable and not the result of something the biological parents did before or during pregnancy. To learn more about your risks of having a child with a genetic condition, talk to your healthcare provider about genetic testing.
Advertisement
If you notice your child has signs of Prader-Willi syndrome, visit their healthcare provider. It’s especially important to see their provider if they miss developmental milestones during infancy. With an early diagnosis, your child’s provider can help you manage your child’s condition, help them meet developmental milestones and manage their diet to reduce complications from the condition.
It may be overwhelming to learn that your child has a rare genetic condition without a cure. Your child’s care team will offer support and guidance so you can give your child the care they need as they grow and develop. Your child may need more time than others their age to reach their milestones. They’ll also need supportive care throughout their life to prevent complications. If you have questions about your child’s diagnosis or how to best care for your child, talk to your child’s provider.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your child shows signs of Prader-Willi syndrome, it’s time to get things checked out. Cleveland Clinic Children’s expert providers are here to guide you through every step.
