Bariatric surgery is a treatment for obesity. Your provider may recommend it if other methods haven’t worked. It changes how your body digests food and helps control hunger. It can improve your health and reduce your risk of obesity-related complications. The surgery takes planning and commitment. But it can lead to lasting results.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
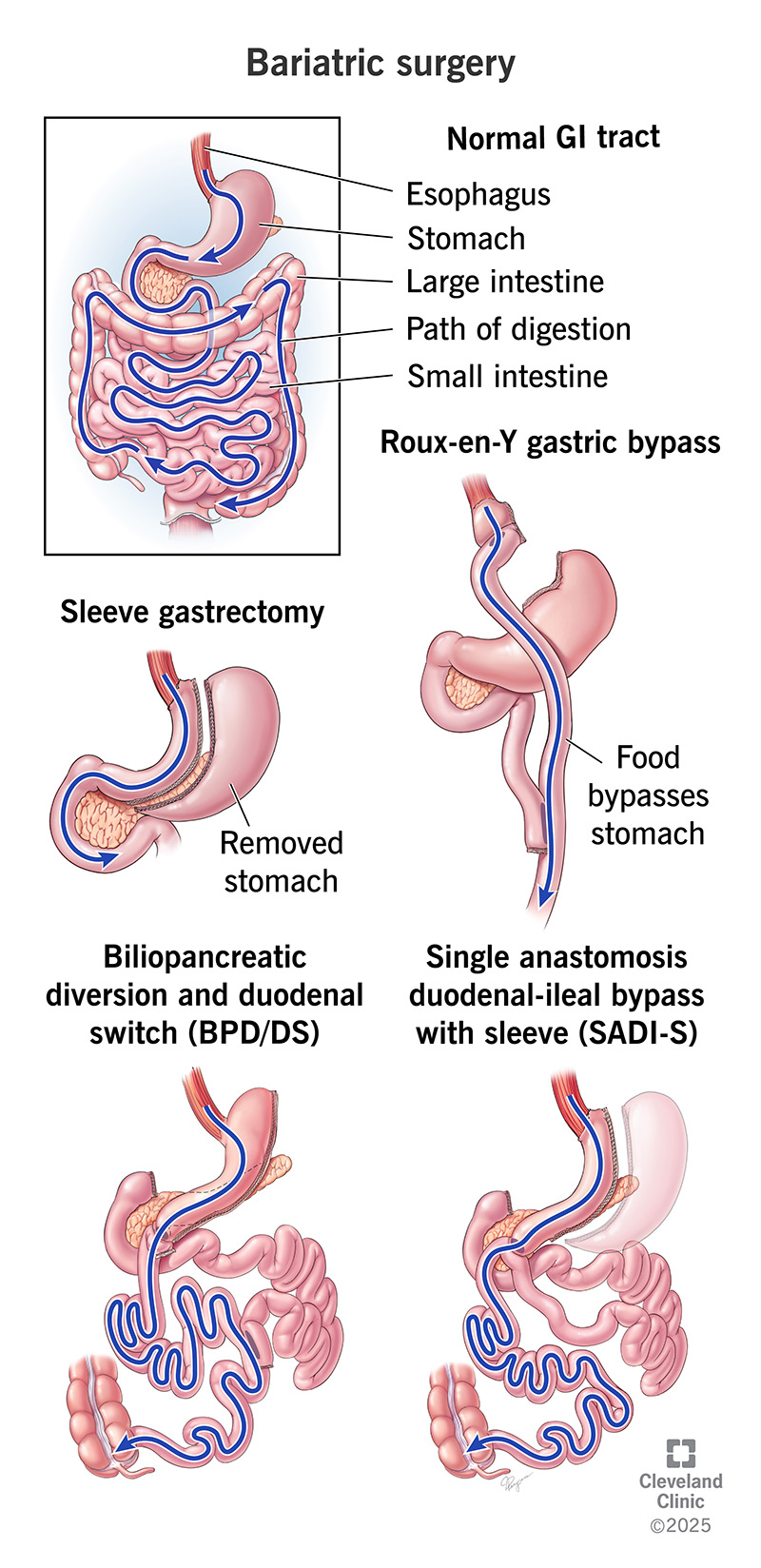
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/bariatric-surgery.jpg)
Bariatric surgery (weight loss surgery, or metabolic surgery) is an obesity treatment. Your healthcare provider may recommend it if other weight loss methods haven’t worked for you. They may also suggest it if you have a high risk of obesity-related complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Bariatric surgery works by making changes to your digestive system. These changes restrict how many calories your body can consume and absorb. The surgery also reduces the hunger signals that travel from your digestive system to your brain. Together, these changes allow your body to maintain weight loss by eating healthy and getting regular physical activity.
Weight loss surgery isn’t a “quick fix” — you’ll need to prepare beforehand and make long-term changes afterward for it to be successful. But if you’ve tried everything else and your provider recommends it, bariatric surgery may be just what you need.
Bariatric surgery requirements begin with a diagnosis of class III obesity. That means you either:
Healthcare providers can easily measure your BMI. It isn’t perfect, but it’s currently the best way to predict weight-related complications. You may need medical tests to diagnose any obesity-related health conditions.
Advertisement
Obesity is linked to many long-term (chronic) diseases. The symptoms of these conditions may greatly improve after surgery and weight loss. If you’re a candidate for bariatric surgery, you may have or be at risk of developing:
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_ordsik0b/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn more about bariatric surgery from Rickesha Wilson, MD.
Before scheduling surgery, your healthcare provider will want to ensure that you’re healthy enough for surgery. You’ll meet with a team of specialists. You may also need to:
Your healthcare provider will usually perform weight loss surgery through a minimally invasive method. That means they’ll make small cuts (incisions) instead of one long cut (open surgery). With this technique, you’ll have:
There are several types of bariatric surgery. Your surgeon will recommend the best type for you. They’ll use factors like your BMI, other health conditions and risks of each type to decide.
Bariatric surgery options include:
Sleeve gastrectomy (gastric sleeve) is the most common type providers use. Your surgeon removes about 75% of your stomach. That leaves behind a narrow tube, or sleeve, about the size of a banana. This restricts how much food your stomach can hold.
Roux-en-Y gastric bypass is another common type providers use. Your surgeon creates a small pouch in your stomach. Then, they connect it to the lower part of your small intestine. Food will bypass the rest of your stomach and go straight to your intestine. This makes you feel full faster.
Biliopancreatic diversion with duodenal switch (duodenal switch) combines a sleeve gastrectomy with an intestinal bypass. It goes around most of your small intestine. That reduces hunger hormones and limits the amount of food your stomach can hold. It also restricts how much nutrition your small intestine can take in.
Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) is a modified version of the duodenal switch. It begins with a sleeve gastrectomy. But then, it bypasses only about half of your small intestine. That allows your intestine to absorb more nutrients.
After surgery, you’ll likely spend a few days recovering in the hospital. For at least the next year, you’ll see your healthcare provider regularly for follow-up visits and testing. They’ll order blood tests to monitor your health. They’ll also screen you for any nutritional deficiencies.
Advertisement
Healthcare providers consider weight loss surgery successful if you lose 50% of any excess weight and maintain a healthy target weight. By this standard, the success rate is more than 90%. Many people experience steady weight loss for the first two years. Then, they stall or regain some weight after that. Usually, the weight regain is less than 25%.
Bariatric surgery has many potential benefits. These include:
Your healthcare provider will help you weigh the pros and cons of surgery. You’ll want to consider the risks of the operation and possible side effects that may occur afterward.
All surgeries involve certain risks. Longer and more complex operations may involve more. Risks may include:
Advertisement
Surgeries that change your digestive system can cause digestive complications. These are sometimes called post-gastrectomy syndromes. Possible side effects may include:
After surgery, you’ll spend a few weeks recovering at home. You may need to avoid intense physical activity for up to six weeks. It may take up to 12 weeks before you can start eating regularly again. Your healthcare provider will tell you what to expect during your recovery.
After a year, you may want to talk to your surgeon about body contouring. Body contouring can help remove excess skin folds and tighten loose tissues. This can be an option if you’ve achieved your target weight and haven’t had any complications.
You may experience rapid weight loss between 12 and 15 months after surgery. You’ll likely reach your lowest weight between one and three years after surgery.
Bariatric surgery can be a game-changer if you have class III obesity. It’s a big decision. But it may help you feel more in control of your health. It’s not about taking the easy way out. It’s about choosing a new way forward when the old ways haven’t worked. Surgery is just one piece of the puzzle. Bariatric surgery can improve your health both now and for the rest of your life.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have obesity and losing weight is an uphill battle, Cleveland Clinic experts can help you decide if bariatric surgery is an option.
