An anastomotic leak occurs when a surgical anastomosis fails and contents of a reconnected body channel leak from the surgical connection. It’s one of the most serious complications of bowel resection surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
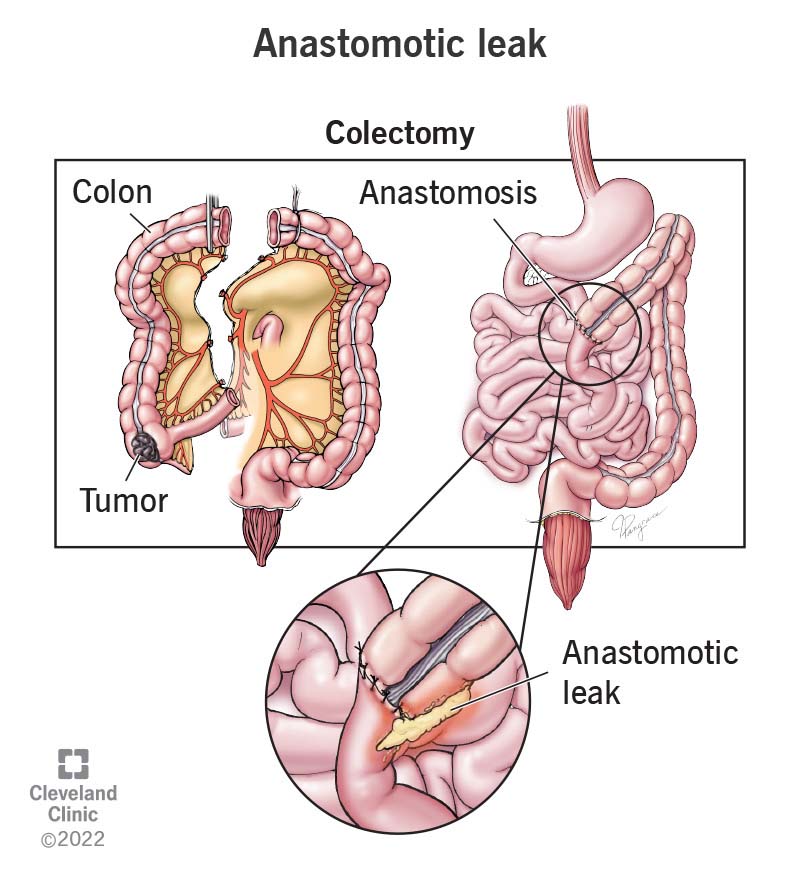
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22324-anastomotic-leak)
An anastomotic leak is a potentially dangerous complication of anastomosis, a surgical procedure. Anastomosis connects two ends of a channel (a tube or passageway) together. It’s usually done after part of the channel has been removed (resected). For example, if you have surgery to remove part of your intestines (bowel resection), the two severed ends of the intestine are reconnected. This connection is called an anastomosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An anastomotic leak is a potential complication of this procedure. It occurs when the two ends of a channel that have been connected together don’t seal completely, and contents from the inside leak out. It’s serious because the channels in our bodies are designed to carry substances that don’t belong in other parts. For example, digestive contents in your gastrointestinal tract contain bacteria that can infect the abdominal cavity if they leak out.
A bowel resection is just one type of operation that involves anastomosis and anastomotic leaks. But it is the most common one. When bowel contents leak into your abdominal cavity, they can cause infection and inflammation of the peritoneum, the tissue that lines your abdominal cavity (peritonitis). Infection in your abdomen can spread to other abdominal organs and can enter your bloodstream. Serious infection can lead to sepsis, a life-threatening physical reaction that can include shock, organ failure or death.
Another body channel that can leak into your abdominal cavity is your urine channel. Any operation that removes one of the organs connected to your ureter, such as a kidney transplant or a prostatectomy, requires anastomosis. If it leaks, urine can collect inside of your abdominal cavity (urinoma). Infection and sepsis are also risks outside of your abdominal cavity. For example, an anastomotic leak in your esophagus — which is part of your gastrointestinal tract — can infect your chest cavity.
Advertisement
A leak may be present at the time of surgery, though surgeons can screen for leaks at this time. It’s more likely to occur sometime during the healing process. Most leaks show up within the first week after surgery, but some may occur later. Healthcare providers keep watch for leaks in the weeks following surgery. Smaller, slower leaks may take longer to show their effects. A delayed anastomotic leak, occurring more than 30 days later, is uncommon.
Anastomotic leaks are reported in about 5% of anastomosis surgeries. About 75% of anastomotic leaks are associated with colectomy, removal of some part of your colon. They’re most common when the resection is located toward the end of your large bowel (in your rectum or sigmoid colon). This part is narrower and more technically difficult to operate on, especially in men.
Technically, anyone who has had anastomosis surgery can suffer the complication of an anastomotic leak. But certain risk factors seem to increase the likelihood of having one.
Risk factors include:
A leak in an anastomosis typically results from a failure in the healing process. There’s no one direct cause, but several factors might contribute. For example:
Advertisement
The first and most common symptoms are:
More advanced symptoms may include:
During your visits with your healthcare provider following surgery, your healthcare provider will assess your condition carefully. They’ll check your vital signs, bloodwork and bowel function on a regular basis. If you show any signs of infection, or if your bowels aren’t functioning right following colorectal surgery, your healthcare provider will consider the possibility of an anastomotic leak. They’ll use imaging tests to investigate — usually, a CT scan with contrast dye.
You’ll be treated immediately with antibiotics to control infection. After that, your treatment will depend on the extent of the leak and how advanced your condition is. It may include:
Advertisement
Hospital stays for anastomotic leaks can be upwards of four weeks.
Leaks that are found can usually be repaired, but early diagnosis and intervention are important for managing infections and controlling sepsis. In general, people who suffer anastomotic leaks are more at risk of further health complications and mortality (death) down the road. It’s not clear how many of these outcomes result from the anastomotic leak, or whether the leak is a symptom of low health status in general.
Many variables contribute to anastomotic leaks, and many of them can’t be changed, including the health status of the people being treated, the difficulty of the particular operation and what happens during the healing process. However, surgeons can screen for leaks that may have occurred at the time of surgery.
Tests to screen for leaks following anastomosis include:
Advertisement
Screening at the time of surgery won’t prevent all leaks, but it can reduce their number and can highlight people who may be more at risk of a recurring leak.
In the case of intestinal surgery, surgeons may be able to prevent the worst effects of a bowel leak by keeping poop out of your bowels during healing. They can do this by creating a temporary colostomy or ileostomy to divert your bowel contents away from the connection and into a bag. This won’t prevent an anastomotic leak, but it will prevent bowel contents from infecting your abdominal cavity if a leak occurs.
Ostomies create a new, artificial opening for poop to come out, called a stoma. This allows your bowels to rest and heal without the irritation of poop passing through. Surgeons create temporary, preventative ostomies under certain conditions. Temporary ostomy surgery is recommended as a preventative measure when people are at higher risk of an anastomotic leak.
If you’re recovering from anastomosis surgery, stay close in touch with your healthcare provider and report any unexpected symptoms. Seek immediate medical attention for any signs of infection, such as:
If you need to have anastomosis surgery and you’re worried about anastomotic leaks, you can ask your healthcare provider about your personal risk factors, what preventative measures they might take and what kind of intervention they might recommend for you. For instance:
If you need anastomosis surgery, it’s probably a life-saving intervention. Under these circumstances, it can be difficult to also consider the possibility of a life-threatening complication resulting from the surgery. As much as healthcare providers dread it, an anastomotic leak is always possible. In general, though, the risk is low, and with awareness and early intervention, most cases can be managed.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Sometimes you have surgery planned. Other times, it’s an emergency. No matter how you end up in the OR, Cleveland Clinic’s general surgery team is here for you.
