Metastasis happens when cancer cells break off from the original tumor, enter your bloodstream or lymphatic system, and then spread to other areas of your body. Doctors can’t cure most metastatic cancers, but treatment can help manage your symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
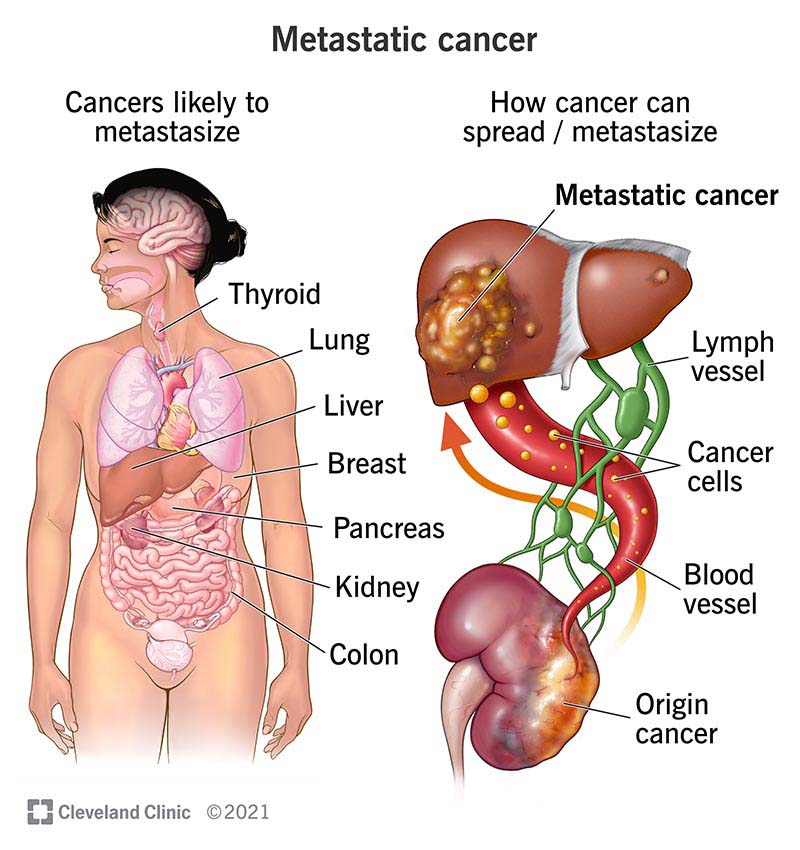
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22213-metastatic-cancer)
Metastasis is when cancer spreads beyond the place where it started to other areas of your body. Nearly all cancers have the potential to metastasize. But whether they do depends on several factors — like the type, size and location of the primary tumor (where the cancer originated).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Metastases can occur in three ways. Cancer cells can:
Other names for metastasis include:
Nearly all cancers can metastasize (spread). Some of the most common types include metastatic:
Where cancer spreads during metastasis depends on the location of the primary (original) tumor. Some of the most common sites of metastases are the:
Metastasis doesn’t always cause symptoms. Cancer cells can grow and spread gradually over many months or years. In some instances, it’s possible to have Stage IV (4) cancer and not know it.
General symptoms of metastasis may include:
Some signs of metastatic cancer depend on the location of the primary tumor and where the cancer cells spread. Depending on the type of metastasis you have, symptoms might include:
Advertisement
Metastasis happens when cancer cells break off from the original tumor and spread to other parts of your body. These cancer cells can travel through your bloodstream or lymph vessels.
Many factors can trigger metastasis, like:
Some people already have metastatic cancer at the time of their diagnosis. In these cases, a healthcare provider usually detects metastases during initial testing.
Other people develop metastases after completing treatment for non-metastatic cancer. During routine follow-ups, a healthcare provider checks for signs of recurrence (cancer that comes back after treatment).
Your healthcare provider may use one or more of the following to diagnose metastatic cancer:
Healthcare providers can treat metastasis based on where the cancer started. For example, if a person has breast cancer and the cancer spreads to their liver, their provider will still treat it the same way as breast cancer. This is because the cancer cells haven’t changed — they’re just living in a new place.
Metastatic cancer treatments may include:
Some metastases may require local targeted therapy to manage symptoms. For instance, if you have breast cancer that spreads to the bone and causes pain or fractures, your provider can treat and ease those symptoms with surgery or radiation to the bone.
Your healthcare provider will work closely with you during cancer treatment and beyond. You’ll likely have many medical visits and will need to make important decisions regarding your overall health. Be sure to lean on friends, family and your healthcare team for support.
In most cases, metastatic cancer isn’t curable. But treatment can slow tumor growth and ease many of your symptoms. It’s possible to live for several years with some types of cancer, even after metastasis. Some metastases are potentially curable, including melanoma and colon cancer.
Advertisement
The five-year survival rate depends on the type of metastases you have. For example, the five-year survival rate for metastatic lung cancer is 9%. This means that 9% of people diagnosed with metastatic lung cancer are still alive five years later. Meanwhile, the five-year survival rate of metastatic breast cancer is 30% for women and 19% for men.
It’s important to understand that survival rates are only estimates. They can’t tell you how you’ll respond to treatment or how long you’ll live. Ask your healthcare provider about survival rates for your specific condition.
You can’t always prevent cancer from spreading. But when providers can detect cancer earlier, a combination of surgery and adjuvant therapy might lower your risk for developing metastasis. Common adjuvant therapies include chemotherapy, targeted therapy and immunotherapy.
Experts continue to research ways to slow, stop or prevent the spread of cancer cells. But sometimes, metastasis happens, despite doing all the right things. According to research, there aren’t any diets that make people more prone to cancer or prevent metastasis from happening.
If you have metastatic cancer, it’s important to know that it’s not your fault and that you haven’t done anything wrong.
Advertisement
A metastatic cancer diagnosis comes with many challenges. These challenges vary from person to person, but you might:
Talking with a counselor or social worker can help you cope with these complicated emotions. Managing stress is also an important aspect of self-care. Try practicing meditation or mindfulness, or find other ways to reduce stress and anxiety.
You should call your healthcare provider any time you develop new symptoms. Your cancer care team can adjust your treatment to meet your specific needs.
Learning about your condition can empower you to make informed decisions. Here are some questions you may want to ask your healthcare provider:
Advertisement
A metastatic cancer diagnosis — when cancer has spread from its original source to elsewhere in your body — is one of the scariest things you may ever encounter. If you recently learned that you have metastasis, you’re probably feeling a lot of complicated emotions. While most metastatic cancers aren’t curable, there are treatments that can ease your symptoms and prolong your life. Ask your healthcare provider for resources and consider joining a local support group. Talking with other people who are going through the same thing can offer healing on your journey.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you’re diagnosed with cancer, you want expert and compassionate care right away. At Cleveland Clinic we personalize your treatment to match your needs.
