Hypoxia is low levels of oxygen in your body tissues. It causes symptoms like confusion, restlessness, difficulty breathing, rapid heart rate, and bluish skin. Many chronic heart and lung conditions can put you at risk for hypoxia. Hypoxia can be life-threatening. If you are experiencing symptoms of hypoxia, call 911 or go to the nearest ER.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
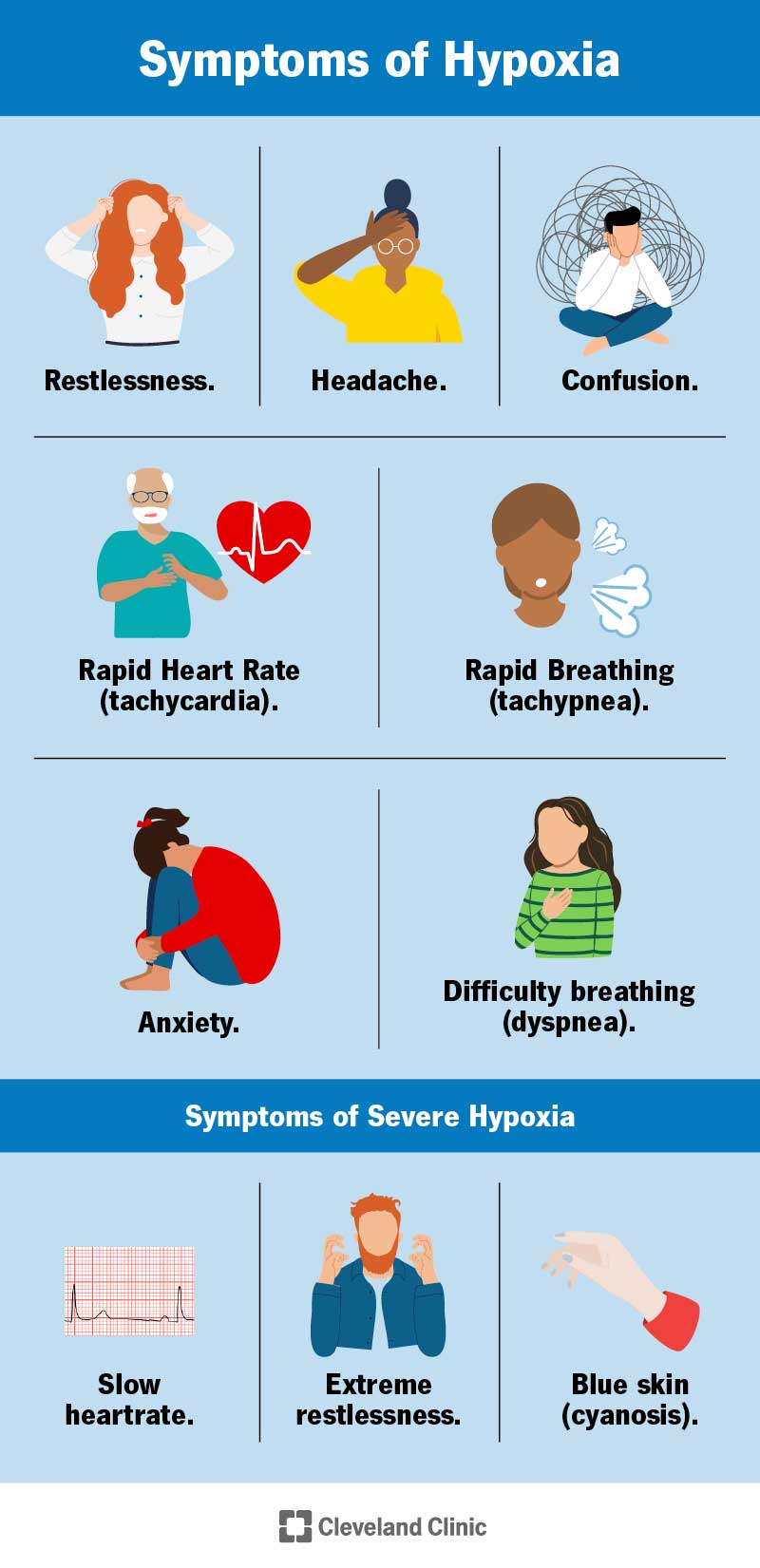
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23063-hypoxia)
Hypoxia is when the tissues of your body don’t have enough oxygen. When you breathe, you take oxygen into your lungs, where it travels through your airways out into small sacks called alveoli. From there, it gets picked up by your blood in small vessels that travel close to the alveoli (capillaries). Finally, it travels through your blood out to other tissues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You can think of oxygen as billions of passengers flying into the airport (your lungs). They get picked up at the gate and get on the highway (blood vessels) to be taken to their destination (your tissues). As the oxygen gets dropped off, it makes room for a different passenger to be picked up: carbon dioxide. Carbon dioxide is a waste product, which is then taken back to your lungs and exits your body when you breathe out.
If not enough oxygen gets through at any place on the journey, it can lead to hypoxia. Airflow and blood flow are both important to the process. This is why lung disease and heart disease both increase your risk of hypoxia. Someone who experiences hypoxia is called hypoxic.
You may hear the words hypoxia and hypoxemia used interchangeably, but they aren’t the same. The names sound similar because they both involve a lack of oxygen but in different parts of your body.
Hypoxia is low oxygen levels in the tissues and hypoxemia is low oxygen levels in the blood. Hypoxia is often caused by hypoxemia but not always. You can be hypoxic but not hypoxemic and vice versa.
Any condition that reduces the amount of oxygen in your blood or restricts blood flow can cause hypoxia. People living with heart or lung diseases such as COPD, emphysema or asthma, are at an increased risk for hypoxia. Some infections, like pneumonia, influenza and COVID-19 can also increase your risk of hypoxia.
Advertisement
Your cells need oxygen to produce energy and help your organs and tissues to do their jobs. While some of your tissues can adjust to temporary dips in oxygen levels, prolonged hypoxia can cause organ damage. Brain and heart damage are particularly dangerous and can lead to death. Lack of oxygen to your brain is called cerebral hypoxia.
Hypoxia symptoms vary depending on the severity, underlying cause and what parts of your body are affected. When your oxygen is low, you might feel like you can’t breathe or think properly. Some hypoxia symptoms include:
Severe hypoxia can cause additional symptoms:
Hypoxia is most often caused by an underlying illness that affects blood flow or breathing. Conditions that can lead to hypoxia include:
For oxygen to make it to the cells in your tissues, you need:
The four types of hypoxia are each caused by a lack of oxygen in any one of these areas.
Low amounts of oxygen in the blood (hypoxemia) can lead to hypoxemic hypoxia, the most common cause of hypoxia. Hypoxemia can be caused by lung and heart diseases, congenital heart defects, and medications that slow your breathing. Traveling to a high altitude, where levels of oxygen are lower, can also cause hypoxemia.
Your blood can have plenty of oxygen, but not enough of it gets to your tissues if the heart doesn’t pump enough blood or there is a blockage in a blood vessel. This is called circulatory hypoxia (also called stagnant hypoxia or ischemic hypoxia). Congestive heart failure and blood clots can increase your risk of circulatory hypoxia.
Anemic hypoxia happens when you don’t have enough red blood cells to carry oxygen from your lungs to other tissues. You can become anemic if your body doesn’t make enough red blood cells or it makes deformed red blood cells.
Advertisement
Histotoxic hypoxia happens when your cells aren’t able to use oxygen properly. In this case, you can have plenty of oxygen coming into your lungs and entering your blood. But when it arrives at your tissues, something keeps your cells from being able to use it. This can happen with cyanide poisoning.
Your healthcare provider will perform a physical exam, including listening to your heart and lungs. They may check your skin, nails and lips to see if they look bluish. Your provider may also order tests to check your oxygen levels and determine the underlying cause of hypoxia, including:
Advertisement
The treatment for hypoxia depends on the underlying cause. The cause might be a one-time event or it could be an ongoing condition. Treatments might include:
If you experience symptoms like confusion, rapid heart rate or breathing, or if you notice your nails, lips, or skin appear bluish, you should seek medical attention immediately. Hypoxia should be treated right away to prevent permanent organ damage. COPD and other medical conditions may cause chronic hypoxia with less severe symptoms. Your healthcare provider will talk to you about managing your specific condition to reduce your symptoms and the risk of your oxygen levels dropping too low.
Advertisement
Hypoxia usually requires medical treatment immediately. Your healthcare provider will talk to you about the underlying cause and how to manage it going forward.
In some circumstances, hypoxia resolves when the underlying condition is treated. In these cases, the need for supplemental oxygen goes away. In other circumstances, you may need chronic supplemental oxygen to ensure there is no ongoing hypoxia or tissue damage from low oxygen levels. Your healthcare provider will discuss your options with you.
The best way to reduce your risk of hypoxia is to manage any underlying conditions that can lower your oxygen levels. If you live with a heart or lung condition, talk to your healthcare provider about your concerns and specific ways to lower your risk. Be aware that certain medications and situations — like traveling to a higher altitude — might increase your risk of hypoxia. Ask your provider about any special precautions you need to take while traveling or changing medication.
If you have an underlying condition that led to — or could lead to — hypoxia, managing that condition is the best way to lower your risk of it happening again.
Hypoxia can be a life-threatening condition. Go to the emergency room if you have any symptoms of hypoxia or if others notice a sudden change in your behavior or awareness (confusion, restlessness, change in consciousness). Go to the ER if you have an ongoing medical condition and your typical symptoms worsen suddenly, or you experience new symptoms that you think might be hypoxia.
If you or a loved one is diagnosed with hypoxia, here are some questions you can ask your healthcare provider:
Hypoxia is a life-threatening condition that is treatable with prompt medical attention. If you have a heart or lung condition that puts you at risk for hypoxia, talk to your healthcare provider about the signs and symptoms to look for and what to do if you think your oxygen is too low. Trust that you know your body best and don’t hesitate to call your healthcare provider or go to the nearest ER if you experience any worrisome symptoms.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Breathing issues can affect your life in many ways. Cleveland Clinic’s respiratory therapy program treats your symptoms so you can feel better day to day.
