A seizure is abnormal electrical activity in your brain. It causes changes in awareness and muscle control. It also causes symptoms that affect your behavior and senses. Seizures can affect anyone at any age and there are a lot of possible causes, from an underlying medical condition to an injury or illness. Treatment options are available to help you manage the frequency and severity of seizure symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
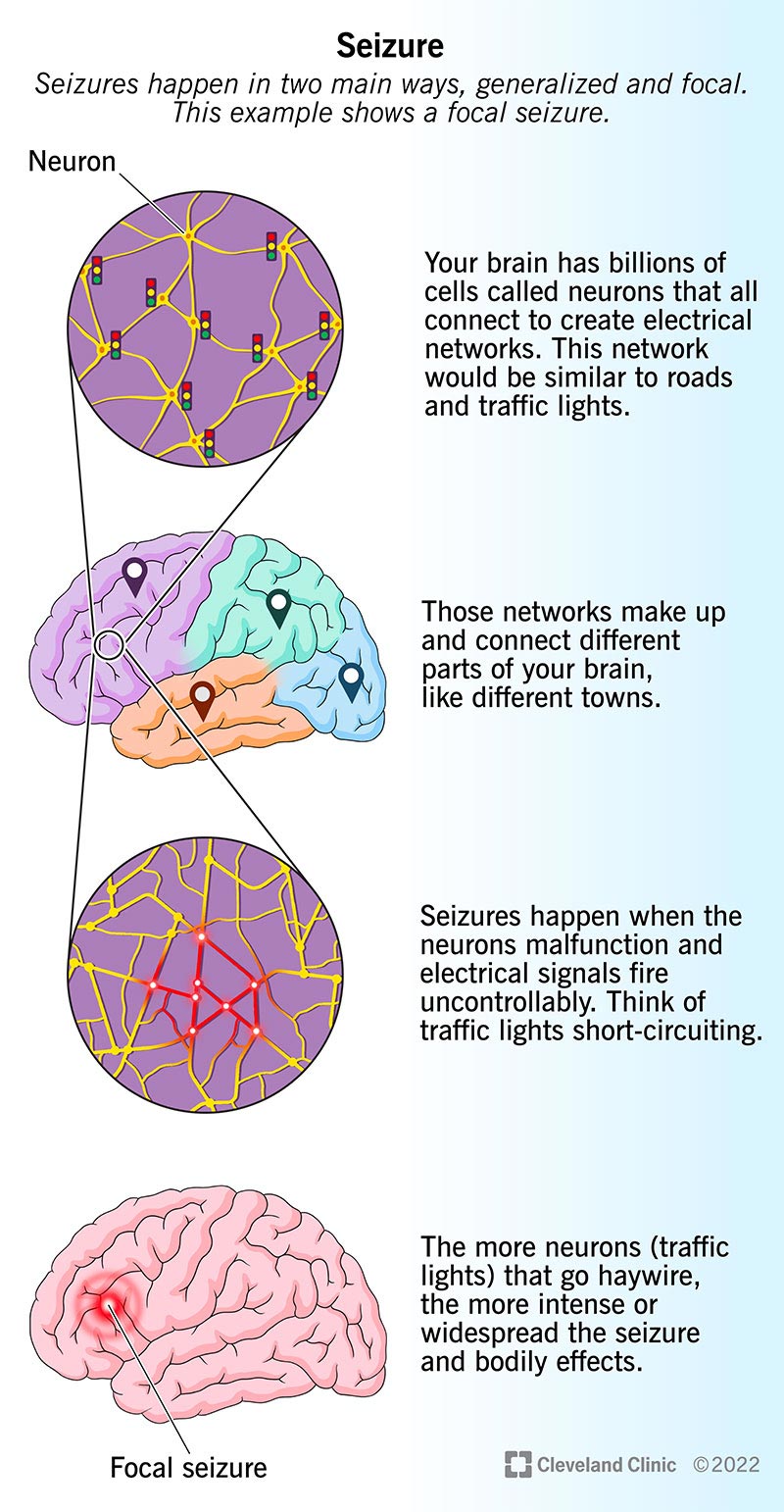
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22789-seizure)
A seizure (pronounced “see-zhr”) is a surge of abnormal electrical activity in your brain. The most recognizable symptoms of a seizure are a temporary loss of consciousness and uncontrollable movements (convulsions).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Not all seizures look the same. You might stop what you’re doing and stare off into space for a few seconds. You might jerk your arm or feel your muscles twitch. You might only have one seizure in your life or have multiple seizures per day. Your experience with seizures can be very different from someone else’s.
There are many possible causes of seizures because a lot of things can interfere with your brain’s typical electrical patterns. These range from changes to your blood sugar levels to an illness, injury or underlying condition.
A healthcare provider can help you find the right treatment for your needs.
There are two main types of seizures:
Advertisement
Generalized seizure types
The types of generalized seizure disorders include:
Focal seizure types
The types of focal seizure disorders include:
Up to 10% of people around the world will have at least one seizure during their lifetimes.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_dp5ajg6r/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn what happens in the brain during a seizure from Dileep Nair, MD.
Seizure symptoms vary based on the type and severity, but may include:
Other symptoms may include:
These symptoms are temporary and only last for a few seconds to minutes.
The stages or phases of a seizure include:
Not everyone who has a seizure experiences all phases, especially the aura. Many seizures come on suddenly and you’re unaware of any early signs.
Advertisement
Warning signs of a seizure may include:
Not everyone experiences warning signs before a seizure.
A surge of electrical activity in your brain causes a seizure.
Neurons (nerve cells) communicate by sending electrical signals to different parts of your brain. When a seizure happens, the affected brain cells fire signals uncontrollably to others around them. This kind of electrical activity overloads the affected areas of your brain and causes seizure symptoms.
Seizure causes fall into two main categories depending on why they happen:
Advertisement
Seizures without a known cause are called idiopathic seizures.
The following may trigger a seizure:
Triggers are different for each person. If you have seizures regularly, you may want to keep track of what you were doing before a seizure took place. A healthcare provider can review this information with you to determine your triggers.
Seizures can happen for many different reasons. These include but aren’t limited to the following:
Other conditions that can cause seizures may include:
Advertisement
Anyone at any age can have a seizure. You may be more at risk if you:
Seizures often involve losing consciousness and passing out. When this happens, there’s a risk of injuries from falling or suddenly stopping what you’re doing at the time (like driving, operating machinery or climbing heights). Convulsions may cause you to smack your arms or legs on hard objects, causing cuts, bruises or broken bones.
Status epilepticus happens when a seizure lasts for more than five minutes or you have more than one seizure without enough time between them to recover. Status epilepticus is a life-threatening medical emergency because it can cause brain damage or even death.
Seizures can significantly impact your mental health. It’s also common to have symptoms of anxiety and depression with seizures.
This may happen because seizures are distracting and can pull you away from the activities you enjoy. You may feel anxious or fearful of having another seizure. You may keep yourself up at night worrying about when the next one might happen. You might avoid going out in public or spending time with loved ones if you’re embarrassed about having a seizure in front of others.
Seizures happen outside of your control, so it’s normal to have these feelings. A mental health professional can help you manage how seizures affect your emotional well-being.
A healthcare provider, usually a neurologist, will diagnose a seizure after a physical exam, neurological exam and testing. During the exams, your provider will learn more about your symptoms and review your medical history and family health history.
It often helps to have someone with you during your appointment who witnessed the seizure to explain what they noticed, as you might not remember what happened.
Tests may help confirm whether you had a seizure and — if you did — what might have caused it.
A key part of diagnosing seizures is finding if there’s a focal point — a specific area in your brain where your seizures start. Locating a focal point can help your provider plan for treatment.
Tests to diagnose seizures include:
Providers might also recommend tests if they suspect injuries or complications from a seizure. Your provider will tell you (or someone you choose to make medical decisions for you) what tests they recommend and why.
Seizure treatment varies based on the type, severity and cause. Your healthcare provider may recommend the following:
If certain types of treatment aren’t successful, your provider may recommend changing the foods you eat. A low- or no-carb (ketogenic) diet may reduce how often you have seizures. Studies are ongoing to learn more about the effectiveness of dietary changes in relation to seizures.
Medications can help you manage seizures by:
Common medications for seizures include but aren’t limited to the following:
A healthcare provider will offer regular follow-up appointments after you start taking a new medication to measure its effectiveness. It could take several months before you and your provider find the medication and dosage that’s right for you. Always continue taking your medications as directed, even if you feel better.
Studies show that an estimated 33% of people who take antiseizure medications notice that seizure symptoms completely stop. Another 33% say they see less frequent symptoms after taking antiseizure medications.
Fewer than half of people who have a single, unprovoked seizure will have another. If a second seizure happens, healthcare providers may recommend starting antiseizure medications. For provoked seizures, the risk of having another depends on what caused the first seizure. If it’s treatable, your risk of having another seizure is low (unless you have a repeat of the circumstances that caused the first seizure).
Medications may prevent seizures or reduce how often they happen. However, it sometimes takes trying multiple medications (or combinations of them) to find one that works best.
In some cases, seizures may be more difficult to treat with medications alone. A provider may recommend surgery, following a specific meal plan or other treatment options.
If seizures happen often, your provider can help you take precautions to stay safe. You may choose to wear a medical ID bracelet or carry a medical ID card with you so others will know what to do in the event of a seizure.
Seizure symptoms usually last for a few seconds to minutes, up to 15 minutes. Symptoms can last longer if you have several seizures, one after the other (this is a medical emergency).
Each person’s experience with seizures is different, so the outlook can vary widely. Your outlook may depend on several factors. These include:
Your healthcare provider will have the most up-to-date information on what you can expect. Let them know if you have any questions.
Seizures are unpredictable, so it’s not possible to completely prevent them. The best thing you can do is avoid possible causes or triggers, like managing blood glucose levels or protecting yourself from illness and injury.
You should go to the emergency room if you have a first-time seizure or if you have any event that makes you pass out and you don’t know what caused it. If you’re alone and have what you think is a first-time seizure, you should call or see a provider right away.
If you had one seizure in the past, it’s important to watch for signs of another. If you have a second seizure, seeing a healthcare provider as soon as possible is very important. Seizures cause changes in your brain that make it easier to have more seizures, so early diagnosis and treatment are key.
Calling an ambulance after a seizure may be unnecessary if a person has seizures regularly. However, even if you know why you had a seizure, you may have injuries that need medical attention.
If you have a seizure, you may want to ask your healthcare provider:
Childhood seizures are possible and happen for many of the same reasons why adults have seizures. Common types of childhood seizures and seizure disorders include, but aren’t limited to, the following:
Is it safe to become pregnant if I have seizures?
Yes, it’s possible to have a safe pregnancy if you have seizures. A healthcare provider may recommend frequent checkups to monitor your and the fetus’s health. Some antiseizure medications aren’t safe to take while pregnant, so a provider will offer safer alternatives to help you manage symptoms. Your healthcare provider is the best person to talk to if you have any questions or concerns.
Seizures may seem like events in dramatic television shows or movies, but they could be an everyday or frequent occurrence for you or a loved one. They’re unpleasant to experience and even scarier to watch. You may not feel like yourself before, during and after a seizure and you’ll likely need time to recover.
Even though seizures are out of your control, a healthcare provider can help you get ahead of symptoms. Your provider may recommend management techniques for an underlying condition, or they’ll help you find ways to identify and avoid triggers. Medications can be very helpful to reduce recurring seizures and surgery may be an option if other treatment types don’t work well.
If you have any questions about what to expect or how to keep yourself or a loved one safe in the event of a seizure, don’t hesitate to contact a healthcare provider.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Epilepsy and seizures can impact your life in challenging ways. Cleveland Clinic experts can help you manage them and find relief.
