Functional seizures (FS), also known as psychogenic nonepileptic seizures or PNES, are attacks that resemble epilepsy-related seizures. They happen due to psychological distress, not abnormal electrical activity in your brain. You can manage FS with cognitive behavioral therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Functional seizures (FS), also known as psychogenic nonepileptic seizures (PNES), are episodes that look and feel like seizures caused by epilepsy. But they aren’t caused by abnormal electrical activity in your brain. Instead, these seizures are a physical reaction of your nervous system to:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you have this condition, the seizures you have are real. You aren’t “faking” it. You don’t have any conscious or voluntary control over these episodes. They can be very disruptive to your life. But help is available.
You may hear your healthcare provider refer to this condition as functional neurological disorder (FND). This is because your symptoms can be explained by functional disruption in your brain’s communication system. Functional seizures are sometimes understood as a problem with the software rather than the hardware of your brain.
Other names for this condition include psychogenic nonepileptic attacks, episodes or spells.
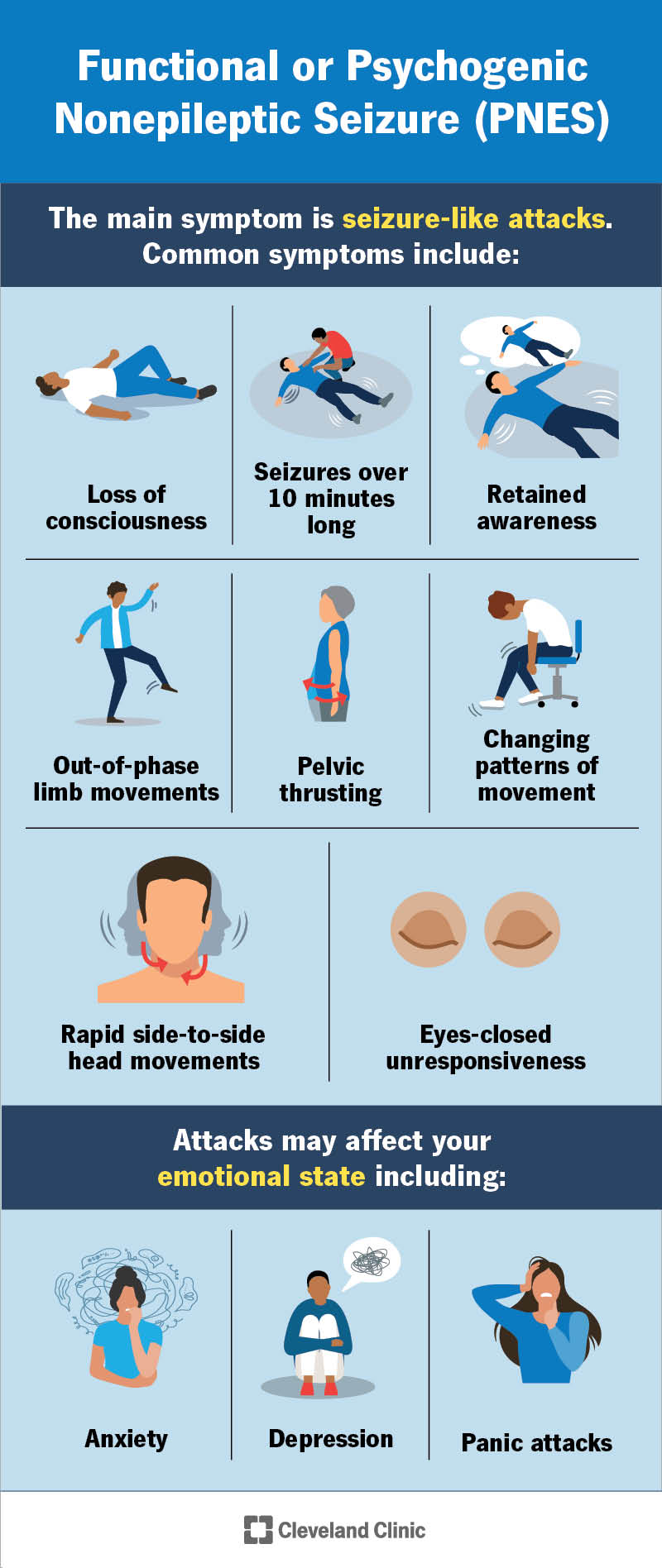
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/psychogenic-nonepileptic-seizure)
The main symptom of FS is seizure-like events (or episodes). These events can look different from person to person.
It may look like you’re having symptoms similar to tonic-clonic seizures, with full-body shaking that’s common in epilepsy. Or you may have twitching or jerking in your limbs. Events may also present as absence seizures (a brief lapse in awareness) or drop attacks. The difference is that there aren’t any abnormal brain waves causing the seizures.
Advertisement
Common symptoms of PNES include:
In addition to seizure episodes, you may experience other symptoms from underlying mental health conditions, like:
Researchers believe FS symptoms are caused by a mix of stress that affects your body, mind and relationships. This is known as the biopsychosocial model.
In addition, the following personal challenges may be contributing factors:
Genetics may also play a role in how this condition develops.
An underlying mental health condition may trigger these seizures. Common conditions include:
You may be more at risk of developing this condition if you:
PNES most commonly begins in young adulthood, but it can start at any age.
You may have little to no awareness or knowledge of when a seizure happens. For this reason, you could be at risk of accidents and injuries that could be potentially life-threatening in certain situations.
Before you know it, you may isolate yourself and stay away from others out of fear or embarrassment. This can pull you away from your loved ones, friends and the activities you once enjoyed.
Having seizure-like episodes may also significantly affect your mental health. FS increases your risk of developing suicidal thoughts. If you’re having suicidal thoughts, know that there’s someone available who can help you. You can call or text 988. This is the Suicide & Crisis Lifeline (U.S.). You don’t have to be in a crisis to ask for help.
Diagnosing PNES can be difficult because symptoms look very similar to epilepsy. Your healthcare provider will make an official diagnosis by recording a seizure or an episode with a video EEG (electroencephalogram).
Advertisement
An EEG measures and records your brain’s electrical signals. During an EEG, a technician places small metal disks (electrodes) on your scalp. The electrodes attach to a machine that gives your provider information about your brain’s activity.
If your episodes are functional, an EEG will show normal electrical brain activity during an episode. However, in those who have epilepsy, EEG will show abnormal electrical activity during a seizure.
Many people with these seizures first receive a misdiagnosis of epilepsy. It’s also possible to have both epileptic and functional seizures in rare cases.
Studies show that cognitive behavioral therapy (CBT), a type of psychotherapy, is most effective in treating PNES.
Your provider will also help you manage any underlying conditions that may trigger episodes. This might include taking an antidepressant in addition to therapy, as directed by your provider.
Antiseizure medications aren’t effective at treating functional seizures.
Cognitive behavioral therapy is a counseling approach where you learn about your mind and body’s reaction to various triggers. You’ll also learn how your thoughts affect your emotions and behaviors. A mental health professional can help you identify and modify unhealthy thoughts, emotions and behaviors to cope with stressful events more effectively.
Advertisement
Your provider may recommend other types of counseling approaches to manage episodes or emotional challenges if CBT isn’t right for you.
During your counseling treatment, you’ll meet your provider regularly. Together, you’ll learn more about how your thoughts affect your emotions and seizures. Then, you’ll set and work on achieving goals. When managing functional seizures, you may have some of the following goals:
It’s OK if your goals don’t match these exactly. Everyone’s goals are unique to fit their needs.
For adults, your provider may suggest a counseling program called neurobehavioral therapy. This is counseling that uses a workbook and is similar to taking a class. You’ll participate in weekly appointments involving 45 minutes of counseling. You’ll do practice assignments at home. This involves activities like journal-keeping or engaging in a social event. Each week, you can build on what you learned until you’ve mastered specific skills.
Advertisement
Counseling can bring up a lot of feelings that you hide away or try not to think about. If you feel overwhelmed with your emotions or feel unsafe, know that your counselor is there for you to help you in this journey. It’s important to contact your healthcare providers to help you or address any questions you may have about your treatment.
PNES may impact your life. But with a proper diagnosis and treatment, symptoms may improve. Some people report no to fewer seizures after following their provider’s guidance and actively participating in counseling. Your provider can give you the best information on what you can expect in your situation.
Learning that stress plays a part in why you experience functional seizures can be stressful! But it doesn’t have to be. Your care team is available to help you understand your diagnosis in a judgment-free environment. Together, you can come up with a treatment plan to help reduce your symptoms and treat any underlying mental health conditions.
Your providers may encourage you to practice the skills you learn in counseling between sessions. Like anything in life, the more effort you put in, the more you’ll get out of it. Building new skills takes time, so don’t worry if you don’t get it right away. Your providers will support you every step of the way.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you’ve been diagnosed with psychogenic nonepileptic seizures, you might have questions. Cleveland Clinic’s expert neurology and psychology providers have answers.
