Frontotemporal dementia (FTD) is a progressive brain disease. This means it gets worse over time as parts of your brain stop working. Depending on where it starts, it can affect your behavior, movement and ability to speak and understand others. There isn’t a cure, but your provider can help you manage symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
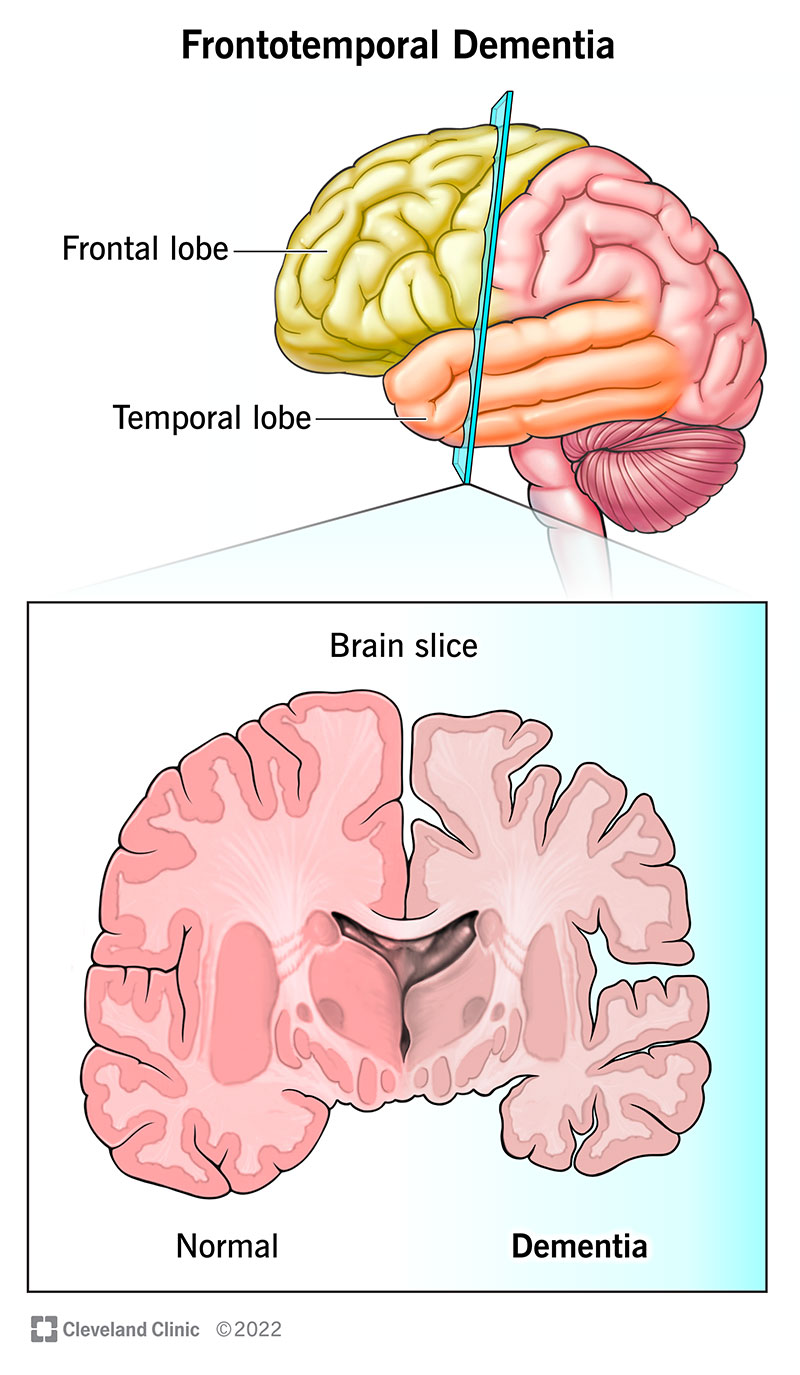
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21075-frontotemporal-dementia)
Frontotemporal dementia is a neurodegenerative disorder that affects the frontal and temporal lobes of your brain. It happens when there’s damage to nerve cells (neurons) in these parts. As it affects more cells, your frontal and temporal lobes shrink.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Symptoms target your behavior, movement, personality and/or language. It’s a progressive disorder. This means that symptoms get worse over time.
A healthcare provider can help you manage symptoms for as long as possible.
The types of FTD include:
The symptoms of FTD vary by type and the part of your brain it affects. They may include:
Advertisement
Symptoms may start mild and will get worse over time.
This condition happens when nerve cells (neurons) in your brain die. Proteins group together within the cell and damage it. As your neurons lose function, parts of your frontal and temporal lobes shrink. This leads to symptoms of FTD.
Studies show that there may be a genetic variant that causes some cases of the disease. This is a change to the instruction manual that your DNA uses to do a specific job in your body.
In other cases, the exact reason why FTD happens isn’t fully understood. Research is ongoing to learn more.
You may be more at risk of developing FTD if:
As FTD gets worse, you may have the following complications:
Severe symptoms may require full-time care to keep you safe and help you meet your needs.
A healthcare provider will diagnose frontotemporal dementia based on your medical history and a physical and neurological examination.
It can be challenging to diagnose FTD. That’s because symptoms may look like other conditions. Tests help rule these out. Your provider may offer the following:
Each type of FTD has its own staging system. Your provider will review your symptoms and identify how severe they are when they make a diagnosis. Most staging includes mild, moderate and severe, among other classifications. Stages will change as the condition gets worse.
There isn’t a cure for FTD. There are treatment options available for managing symptoms. These vary by the type of frontotemporal dementia and the symptoms you have. Your provider may recommend:
FTD changes how your brain works. This means that some of the things that you used to be able to do will become harder as the disease affects more of your brain. Over time, you may need full-time care. This is to help you complete your daily routine since living independently can be unsafe.
Advertisement
If you have an early diagnosis of FTD, you may want to talk to your loved ones or to anyone you trust to make important decisions for you. These conversations help your caregivers honor your wishes if you can’t make choices on your own in the future.
While these conversations may feel difficult, having them sooner can help avoid confusion in the years to come. They also mean your loved ones won’t face the painful, difficult situation of having to guess what you want.
Also, you should put your wishes and decisions in writing. That includes preparing documents connected to legal issues and what happens if you can’t make decisions for yourself.
Your healthcare provider can tell you more about what to expect. They can also direct you to resources and services that might help you.
The average life expectancy after a diagnosis of FTD is seven to 13 years after symptoms start. This varies from person to person and by type. Your provider is the best person to talk to about your situation because it may or may not match statistics.
While this condition isn’t fatal on its own, it often causes other issues that are serious or even life-threatening. One common issue is trouble swallowing. This causes problems with eating, drinking and speaking. It increases the risk of developing pneumonia or respiratory failure.
Advertisement
Frontotemporal dementia can be a devastating diagnosis to receive. Not only will it impact you, but it can have a significant impact on your loved ones, as well. As symptoms get worse, you could lose your ability to control your behavior and movement. It may even impact your ability to speak and understand those around you. This can be scary, frustrating and emotionally draining.
When a diagnosis happens, it’s important to work with your care team. Put your wishes or instructions about your future into writing as soon as possible. The effects of FTD will impact your ability to make decisions and take care of yourself. These documents will be helpful in the years to come. If you have any questions or concerns, a healthcare provider can help you.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Frontotemporal dementia can change your life. Cleveland Clinic is here for you and your family, offering care and support for all types of dementia.
