Functional neurological disorder (FND), formerly conversion disorder, is a condition in which a mental health issue disrupts how your brain works. This causes real, physical symptoms that you can’t control. Symptoms can include seizure-like attacks, muscle weakness or reduced senses. FND is often treatable with different types of therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Functional neurological disorder (FND), formerly known as conversion disorder, is a neuropsychiatric (or brain-based) disorder that affects the way your brain sends, receives and processes messages.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With this condition, the structure of your brain is normal. Scans like CTs usually look healthy. The difference is in how your brain communicates with your body. In FND, the signals can get interrupted, and that leads to real symptoms.
When these signals are mixed up, it can affect your movement, feeling, speech or other body functions. To others, it might seem like you’re faking or seeking attention. This can be extremely frustrating (invalidating) because they can’t see the cause. It can affect both your physical and emotional health.
Another name for this rare condition is functional neurological symptom disorder (FNSD). A team of healthcare providers can help you manage symptoms.
In the past, healthcare providers saw functional neurological disorder as only a mental health disorder. They believed a person “converted” hidden stress or trauma into physical symptoms. That idea gave the condition its old name.
Research now tells us that this name isn’t accurate.
A specific brain scan called a functional MRI can show your brain activity at rest and during specific tasks. These scans reveal that FND changes how your brain sends and receives signals.
Research also shows that people with FND may have unusual activity in brain areas linked to their symptoms. Also, not everyone with FND has a history of trauma or stress.
Advertisement
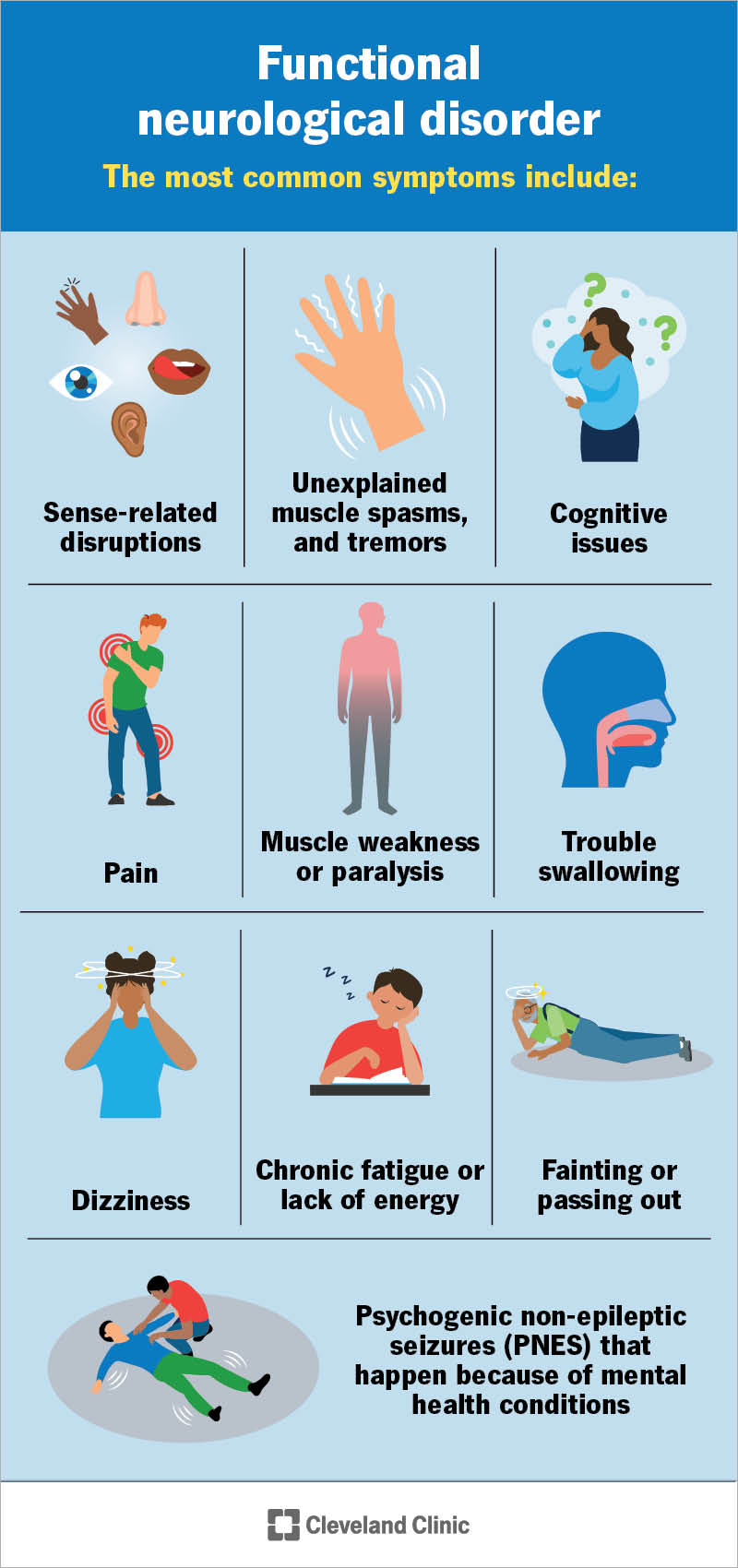
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/functional-neurological-disorder)
Symptoms usually appear suddenly and may interfere with your daily functioning. They might get worse when you pay attention to them and get better when you use distraction techniques.
The most common FND symptoms include:
You might also notice:
Healthcare providers aren’t sure exactly what causes FND. It happens when there’s a problem in how your brain and body communicate.
It’s very common to describe FND as a software issue. Think of your brain as the computer’s hardware, and your nerves as the wires that carry information. The “software” is the program that tells your brain and nerves how to work together. In FND, the hardware and wires are fine, but the software has a glitch. This glitch changes the way your brain sends and receives signals. This can cause a lot of physical symptoms that aren’t otherwise explained medically.
Just like a computer with a software bug, nothing’s broken inside. But things don’t work as they should. Treatment helps “retrain” your brain and nervous system so the signals flow normally again.
Certain situations may trigger FND, including:
Sometimes, instead of stopping, triggers can cause symptoms to cycle on a loop. This happens because your brain gets stuck on them. This pattern can lead to FND. Experts are still studying how and why this happens.
Advertisement
FND can develop at any time, including during childhood. It’s more likely to affect females than males.
You may be more at risk if you have:
You might not have any of these risk factors, but still have symptoms.
FND care ideally consists of a multidisciplinary team of healthcare providers, including, but not limited to, neurologists, psychiatrists, psychologists and physical/occupational/speech therapists.
Healthcare providers use different tests to diagnose functional neurological disorder. It’s a complex condition, and symptoms can look like those of other conditions. This can make it hard to tell them apart.
Getting a diagnosis may feel like a long process with many tests. You’ve likely seen many providers before getting an FND diagnosis. But finding the right care is important.
Once you get a diagnosis, your providers will focus on building trust. You may have gone through a long process to get here. Along the way, people may have even told you that your symptoms were “made up.” That stigma can keep many people from getting care and can affect their mental well-being. But you’ve made real progress by getting this far.
Advertisement
Your care team will reassure you that your symptoms are real and that you’ve done the right things. They’ll explain the condition in detail and answer any questions you have.
The exams and tests your provider offers will depend on what symptoms you have. They may include:
After your provider gets the results of your tests, they’ll use the following criteria to make an official diagnosis:
Functional neurological disorder is complex and requires a multidisciplinary approach. This often includes:
Advertisement
If you have FND, the best thing you can do is work closely with your healthcare provider. They’re here to guide you through treatment and help you find what works best for you. If something feels off or if you notice changes in your body that you don’t understand, reach out. Your care team wants to know what’s going on so they can support you.
The outlook for FND can vary. The condition isn’t life-threatening. But it can affect your mental health and overall well-being. You may have severe symptoms that keep you from working or enjoying your daily activities.
Factors that may improve your outlook include:
Recovery with FND isn’t always a straight path. You may go through times when getting better feels hard. Your symptoms might even get worse before they improve. This is common. But it doesn’t mean you’re failing or that things are hopeless.
Still, it can be complicated as you go through treatment. It’s important to know that help is available if you need it. If you’re in a rough spot or thinking about suicide, call or text 988 (U.S.) to reach the Suicide and Crisis Lifeline. Someone is available to help you 24/7.
FND can last for a short or a long time. If symptoms last fewer than six months, it’s called an acute case. If symptoms last more than six months, it’s called a persistent case.
Getting diagnosed early and starting treatment right away can improve your chances of recovery. For some, symptoms may last for years or even be lifelong, especially if care is delayed or there’s an interruption to treatment.
When your body isn’t working the way it should and no one can explain why, it can feel confusing, exhausting and lonely. Your symptoms are real and disruptive. But unlike many other conditions, they don’t always show up on a scan or blood test. This can make getting a diagnosis harder. But stick with it.
Progress for functional neurologic disorder (FND) may happen in small steps. That could mean gaining more control over your movements, finding a therapist who understands you or feeling supported by your care team. But it takes strength to get this far, and you’ve already shown that. You don’t need to solve everything at once. Each step forward is part of recovery.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Your mental well-being is just as important as your physical well-being. Cleveland Clinic’s mental health experts can help you live life to the fullest.
