Vascular dementia results from conditions that damage blood vessels and block blood flow to your brain. Many of these conditions, like heart disease, diabetes and high blood pressure, are manageable. There’s no direct treatment or cure for vascular dementia, so managing these risk factors is crucial to help prevent it from becoming severe.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Vascular dementia is when there’s decreased blood flow to areas of your brain. Blood provides oxygen and nutrients. A lack of it damages brain tissue. It leads to symptoms that affect daily living, like memory loss, confusion, and personality and behavioral changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Several conditions can cause a lack of blood flow, including stroke.
Vascular dementia is one of the most common types of dementia in people after age 65 in North America and Europe. About 5% to 10% of people with dementia have only vascular dementia. But it often happens along with Alzheimer’s disease. When someone has both, providers call it mixed dementia (having more than one cause of dementia).
You may hear your healthcare providers use the term “vascular cognitive impairment” (VCI) instead of “vascular dementia.” This term covers the full range of thinking changes from vascular damage — from mild cognitive impairment (MCI) to dementia.
Because vascular dementia can look different for each person, your healthcare team can help you understand your diagnosis and what to expect moving forward.
Healthcare providers use different terms for vascular dementia. They reflect the number and type of blood vessels involved and how symptoms develop. They include:
Advertisement
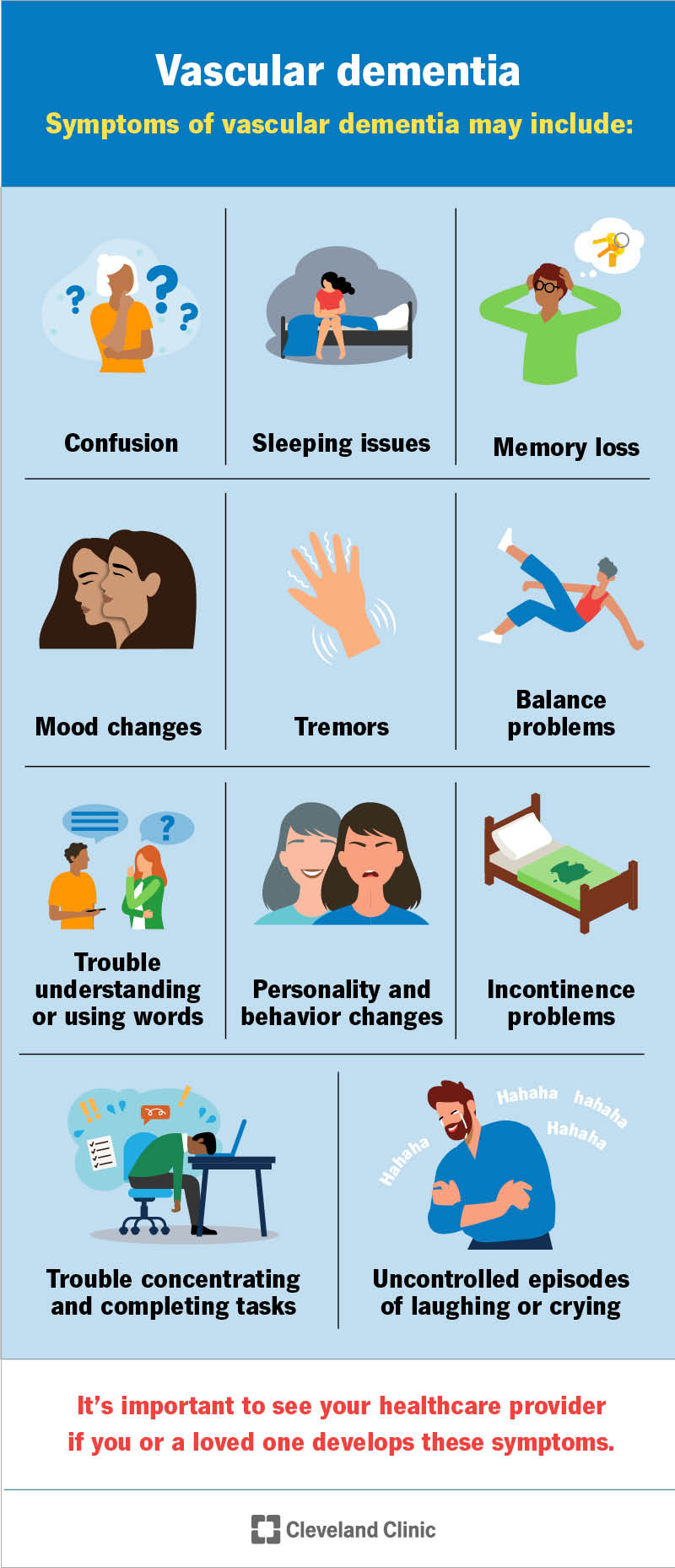
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22216-vascular-dementia)
Symptoms of vascular dementia can vary widely. They depend on which parts of your brain it damages and how severe it is. Symptoms may include:
It’s important to see your healthcare provider if you or a loved one develops these symptoms.
There are no clear stages of vascular dementia. It affects each person differently and progresses in a variety of ways.
Most often, symptoms get worse over many years. But they may be most obvious and sudden after a major stroke. There may even be short periods when symptoms improve. But if more strokes happen, they can cause further decline.
Vascular dementia can also occur along with Alzheimer’s disease. Having both can affect how symptoms change over time.
Conditions that damage blood vessels in your brain or partially or fully block blood flow cause vascular dementia. When blood flow decreases, parts of your brain don’t get enough oxygen and nutrients. Without these, brain cells begin to die.
Common causes include:
Certain factors increase your risk of having blood vessel issues and vascular dementia, including:
Vascular dementia itself isn’t hereditary (passed down through genes). But conditions that raise the risk, like high blood pressure and heart disease, can run in biological families.
Two rare types happen because of gene mutations (changes):
Advertisement
By the later stage of dementia, it will have a severe impact on most aspects of your or your loved one’s life. People in later stages often need full-time care and daily support.
Late-stage or end-of-life symptoms may include:
Your or your loved one’s healthcare team, hospice nurse or palliative care provider is the best to ask about timelines. They can explain what signs to look for and give you a general idea of what to expect.
A healthcare provider needs to evaluate you to confirm a diagnosis. There are many types of dementia, and several symptoms are similar to other conditions.
Your provider will:
Your provider will likely recommend a variety of tests. You may also see dementia specialists, like neurologists and geriatricians, for a diagnosis. The following tests help diagnose this condition:
Advertisement
Healthcare providers use the following criteria to diagnose vascular dementia:
Advertisement
These criteria suggest the greatest likelihood that mild cognitive impairment or dementia is due to vascular damage and not another cause.
Vascular dementia isn’t reversible. Brain damage can’t be fully repaired. Instead, the main goal of treatment is to prevent or slow down further damage by managing risk factors. Treatment also involves helping you find new ways of doing things to make up for brain damage.
Unlike for Alzheimer’s disease, there aren’t any medications that have U.S. Food and Drug Administration (FDA) approval for this condition specifically. But providers may prescribe cholinesterase inhibitors for vascular dementia. Studies show that they may result in slight or modest cognitive improvements by increasing blood flow in your brain.
Memantine is another medication that’s approved for Alzheimer’s disease and may help with vascular dementia.
Your provider may prescribe other medications to help manage risk factors for stroke. These include medications for high blood pressure, high cholesterol and diabetes.
You may work with specialists to manage symptoms of vascular dementia. For example, physical and occupational therapists can help you improve your physical abilities and find new ways of doing everyday tasks. A speech-language pathologist can help with speaking, swallowing and learning other ways to communicate.
Other specialists you may work with include:
These specialists will work with you and your loved ones to make sure you have ongoing care that matches your needs and goals. They’ll help you plan ahead for medical and financial decisions. They’ll also make referrals for palliative care or hospice when vascular dementia progresses to its later or end stages.
You or your caregiver should call your healthcare provider if you notice any new or worsening symptoms. Your provider or care team will want to assess any changes and adjust your treatment plan if needed.
Vascular dementia may get worse over time. The changes can happen suddenly or gradually. Each person has their own unique journey. Treatments may help slow the progress of the disease. You and your healthcare provider will work together to develop a treatment plan best suited for managing symptoms and the stage of the disease.
Lean on loved ones for support during this time. Together, you can make a plan to ensure your quality of life and wishes are respected as dementia progresses.
The life expectancy depends on the severity of the disease. Vascular dementia has wide-ranging severity and affects each person differently.
The life expectancy for vascular dementia is lower than it is for people with Alzheimer’s disease. This is because someone with vascular dementia is more likely to die from a stroke or heart attack than from dementia itself.
Vascular dementia is unique from many other forms of dementia in that it’s partly preventable. There are some risk factors that you can’t change, like your age or genetics. But you can manage many others to try to prevent it — mainly those that damage your blood vessels. Steps you can take include:
If you have any of these risk factors, talk to your provider about what you can do to manage them.
Vascular dementia is one of those conditions that doesn’t always follow a clear path. Symptoms may show up suddenly after a stroke or slowly build over time.
But there are steps you can take to manage symptoms and protect your brain health. Managing risk factors like high blood pressure, diabetes and cholesterol can prevent further damage. And if you or a loved one has this diagnosis, know that there are resources and specialists who can support you in staying as comfortable as possible.
Talk with your healthcare provider about what to expect and how to plan ahead. Having those conversations now can make a big difference later.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
It can be unsettling when your brain stops working like it used to. Cleveland Clinic’s cognitive decline experts help you manage the symptoms and provide support.
