Mitral valve prolapse (MVP) is a common heart issue with floppy valve leaflets that don’t close tightly. It’s harmless for most people, but can become dangerous if it leads to severe mitral regurgitation (leaky valve). People with severe regurgitation may need valve repair or replacement.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
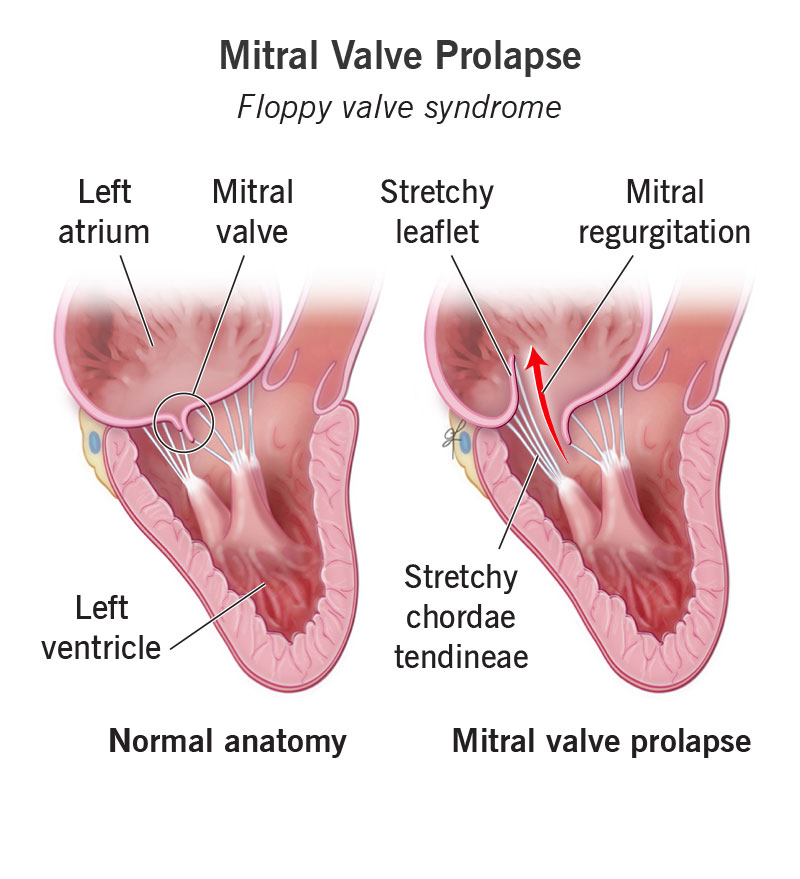
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17241-mitral-valve-prolapse)
Mitral valve prolapse (MVP) is a heart issue in which your mitral valve flaps bow or flop back into your left atrium. This may prevent your valve from closing as tightly as it should between your left atrium and left ventricle. These are the two heart chambers that collect and pump oxygen-rich blood out to your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your mitral valve’s two tissue flaps (leaflets) open and shut with each heartbeat. This is how they manage blood flow out of your left atrium and into your left ventricle.
Mitral valve prolapse is a common form of mitral valve disease that affects 2% to 3% of the general population. MVP is often harmless. Many people have no symptoms and don’t even know they have it. That’s because their valve can still function well.
Some people with moderate or severe prolapse have symptoms and need treatment. It may be daunting to hear that you need surgery. But it may be comforting to know that many people have had successful procedures.
Although most people with this condition don’t have them, mitral valve prolapse symptoms may include:
People who have symptoms of mitral valve prolapse might not have a severe form of the condition. Symptoms and severity don’t always go hand-in-hand when it comes to mitral valve prolapse. Still, it’s important to tell a provider about your symptoms.
Valve tissue weakness (myxomatous degeneration) causes mitral valve prolapse. It’s not always clear what causes this tissue weakness. In some cases, families may pass it down to their biological children. Researchers have linked mitral valve prolapse with several genes, including FLNA, DCHS1, DZIP1 and PLD1.
Advertisement
Some connective tissue disorders may cause myxomatous degeneration. These include Marfan syndrome, Ehlers-Danlos syndrome and Loeys-Dietz syndrome.
Mitral valve prolapse affects people of all ages. Some people are born with mitral valve prolapse, including those who have connective tissue disorders. Rheumatic heart disease, scoliosis and Graves’ disease may also increase the risk of mitral valve prolapse.
MVP is more common in females. But males are more likely to develop severe mitral valve regurgitation (blood leaking backward).
The main complication of MVP is mitral regurgitation. This means blood leaks the wrong way through your valve from your left ventricle into your left atrium. MVP is one of the most common causes of mitral regurgitation. If the leak is severe enough, you may need surgery or a procedure to help your valve work as it should.
People who have mitral valve prolapse and regurgitation are at risk for complications, including:
Healthcare providers diagnose mitral valve disease through a physical exam and tests. A provider can learn a lot by listening to your heart with a stethoscope. If you have mitral valve prolapse, your provider will hear a clicking sound followed by a murmur. “Click-murmur syndrome” is another name for mitral valve prolapse because of its distinctive sound.
During your exam, your provider will also discuss your medical history and family history with you. As mitral valve prolapse sometimes runs in families, this information matters.
If your provider suspects you have MVP or another valve issue, they’ll order at least one test to confirm the diagnosis.
Echocardiography is the main method providers use to diagnose MVP. This test uses ultrasound technology to check your heart’s structure and function. You may need one or both of the following types of this test:
Your provider may order more tests to learn more about your heart. These include:
Many people with mitral valve prolapse don’t need treatment. If you have a mild form, your provider may simply monitor you with regular checkups. They may prescribe beta-blockers to help manage symptoms like dizziness or heart palpitations.
If you have atrial fibrillation or a history of stroke, you may need to take anticoagulants (blood thinners). Talk with your provider about which medications, if any, are right for you.
Advertisement
Surgery or a transcatheter procedure may be the best mitral valve prolapse treatment for some people. The most effective approach depends on many individual factors. Surgical/procedural options include:
The answer is different for each person. Talk with your provider about which treatment plan is best for you. Make sure you understand the benefits and risks of any mitral valve prolapse treatments. The best treatment plan for you depends on many factors, including:
Advertisement
About 1 in 10 people with mitral valve prolapse need to have a surgeon repair or replace their valve. You may need valve repair or replacement if:
In most cases, mitral valve prolapse doesn’t cause problems and you don’t need treatment. Mitral valve prolapse may not harm your body. But in some people, MVP can lead to regurgitation and other issues.
If you have a mitral valve prolapse diagnosis, talk with your provider to learn about the level of severity and what you can expect.
The life expectancy for people with mitral valve prolapse depends on many factors. These include:
Advertisement
Mitral valve repair can help you live just as long as people without valve issues. One study shows that the life expectancy of people who had a repair is the same as the life expectancy of the general population. This was true for people ages 40 to 89.
So, if you have mitral valve prolapse, it’s important to get regular checkups and tell your provider about any new or changing symptoms. This will allow you to get treatment if and when you need it.
People who have severe regurgitation but don’t get a valve repair face poor outcomes. They have a 20% chance of dying within one year and a 50% chance of dying within five years.
Your provider can tell you about your situation and prognosis.
There’s no specific way to prevent mitral valve prolapse. But you can reduce your risk of acquired heart valve disease (valve problems that come up as you get older). Some tips include:
Following these tips can also help you stay strong enough for surgery, should you need it.
Ask your provider how to make changes that feel doable to you. Start small and remember that every small change you make can add up to make a big impact down the road.
Talk with your provider to learn what you can expect and when you should be concerned. It’s common for people with mitral valve prolapse to feel anxiety over their condition. But in many cases, mild symptoms aren’t a reason to worry. Your provider can prescribe medication to manage symptoms like a fast heartbeat or heart palpitations.
But it’s important to recognize symptoms when they happen. No symptom is too small to share with your provider. Even if you think it’s nothing, tell your provider about what you’re feeling. They’ll make sure you get checked when needed so you can feel comfortable going about your daily life.
Some people with mitral valve disease may need to avoid intense activity. It’s essential that you talk with your provider to learn about limits specific to you and your diagnosis. Activity restrictions depend on many factors. These include whether you have:
Many people with MVP don’t have activity restrictions. Check with your provider before starting any new workout plan, just to be safe.
Mitral valve prolapse can get worse as you get older. That’s why it’s important to keep all of your appointments with your healthcare provider. They’ll monitor your valve and discuss treatment options with you if needed.
Valve disease is more common among people who are over age 65. This is partly because of the wear and tear on your heart from daily life. But heart problems like coronary artery disease or heart attacks can also take a toll on your valves, including your mitral valve. This is especially true for people over age 75.
Talk with your provider to learn more about how aging affects your mitral valve.
Your provider will likely recommend regular visits with them, as well as frequent physical activity. You can also avoid things that put stress on your heart, like:
Your provider will let you know how often you need to come in for follow-up visits. It’s important to keep all of your appointments. You may also need regular imaging tests to check on the health of your mitral valve.
Call 911 or your local emergency number if you experience:
If you’re taking blood thinners (anticoagulants) and fall, seek care right away. Blood thinners raise your risk of internal bleeding. Even if you feel OK, it’s important for a provider to check you over. Internal bleeding can be fatal without treatment.
If you just learned you have mitral valve prolapse, you probably have many questions, like:
Mitral valve prolapse is a form of heart valve disease. Heart valve diseases fall under the big umbrella of cardiovascular disease. Cardiovascular diseases are any conditions that affect your heart or blood vessels.
Mitral valve prolapse (“floppy valve syndrome”) is a type of myxomatous valve disease. This means the tissue of your mitral valve leaflets is abnormally stretchy, which makes them floppy.
Mitral valve prolapse (MVP) is a common condition that may not change your life at all. But if it leads to mitral regurgitation (leaky valve), you may feel nervous about having surgery to help your valve work better. Talk with your provider about the risks and benefits of valve repair, and ask about all available options.
If you need valve repair, it’s important to choose a hospital that does these types of procedures every day. High-volume hospitals are prepared to use the latest technology to reduce your risks and give you the best possible outcomes.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Problems with your heart can be scary. Our experts can diagnose and treat mitral & tricuspid heart valve disease.
