Auscultation is a method your healthcare provider may use to listen to the sounds of your heart, lungs, arteries and abdomen. They’ll place a stethoscope directly onto your chest, back and/or abdomen. Your healthcare provider uses auscultation during physical exams to check your circulatory system, respiratory system and gastrointestinal system.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Auscultation (pronounced “AW-skull-TAY-shun”) is listening to the sounds of your heart, lungs, arteries and belly (abdomen). Your healthcare provider will use a stethoscope to listen to the sounds of your body. They’ll place the stethoscope directly onto your chest, neck, back and abdomen, listening for different sounds, quality, volume, timing and more.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Auscultation is a safe and easy way to diagnose potential medical conditions. It’s non-invasive and one of the oldest techniques healthcare providers use today.
Your healthcare provider uses auscultation during routine physical examinations. They want to check the sounds of your circulatory system, respiratory system and gastrointestinal system. They’ll use auscultation to keep an eye on your overall health, or to confirm or rule out various medical conditions.
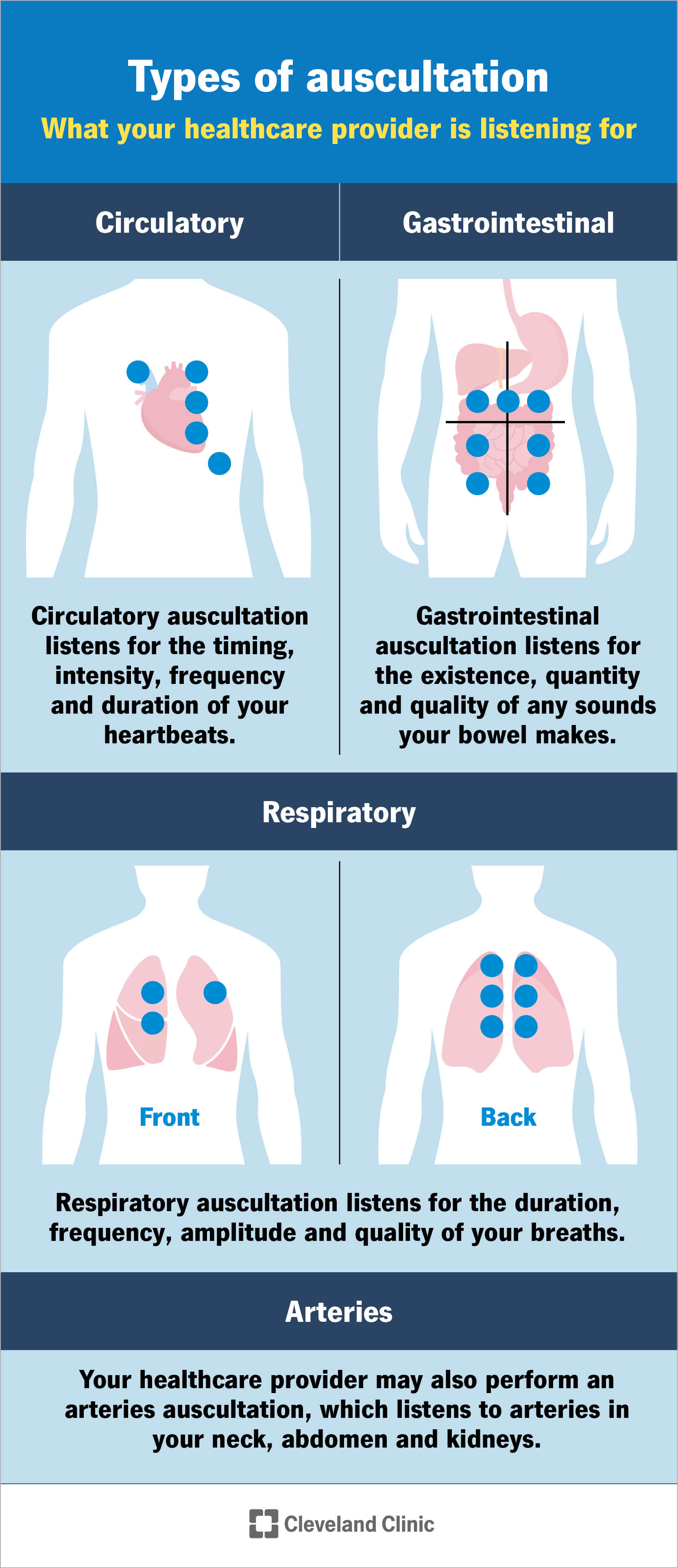
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23080-auscultation)
A healthcare provider may perform auscultation near the body systems they’re listening to.
A healthcare provider will listen to the sounds your heart makes through a heart or cardiac auscultation. To do this, they’ll usually have you sit up or lie comfortably at a 45-degree angle. They may ask you to turn toward your left side or position you in another way to hear your heart clearly.
They’ll place a stethoscope on your chest to listen to your heart sounds. They’ll move the stethoscope to the five areas of your chest where they can hear your heart valve sounds the best. These heart auscultation points are all in your upper left chest area.
Your healthcare provider will listen for:
Advertisement
Your healthcare provider will listen to the sounds your lungs make through a lung auscultation. They’ll ask you to sit upright, if possible. Your provider will place a stethoscope on your chest and ask you to take deep breaths through your mouth. Then, they’ll move the stethoscope to different pulmonary (lung) auscultation points. They’ll start at the top of your lungs and move downward, then compare the sounds of each lung.
After listening to your lungs from the front of your body, they’ll place the stethoscope on your back. Just as before, they’ll start at the top and work their way down, going from side to side. They’ll listen to one complete breath cycle at each auscultation site. After that, they’ll compare the sounds they hear between the front and back of your lungs.
Your healthcare provider will listen for:
Your healthcare provider can also listen to arteries of your neck, abdomen and kidneys, if necessary.
Your provider will listen for:
Your healthcare provider will listen to the sounds your intestines make through abdominal auscultation. You’ll lie down comfortably on your back and prop your head up on a pillow. Your provider may put a positioner under your knees for comfort.
Your provider will place a stethoscope on your abdomen. They’ll move the stethoscope over different regions of your abdomen to listen to the sounds your bowels make.
Your healthcare provider will be listening for:
Normal heart sounds have a steady, two-beat, or “lub-dub,” rhythm to them. The first sound is called S1, or a lub. The second sound is called S2, or a dub. Your healthcare provider can hear these sounds when your heart valves are closing.
Your healthcare provider may hear various abnormal sounds in your heart, like:
Advertisement
The different auscultation points of your lungs produce different normal sounds. Typically, normal lung sounds are soft and hollow. Your provider can hear them when you inhale.
Your healthcare provider may hear various abnormal sounds, including:
Advertisement
Normal bowel sounds make a low-pitched, gurgling noise. The noise occurs every five to 10 seconds as your intestines push food through your system. This means your gastrointestinal (GI) tract is functioning properly.
Your healthcare provider will auscultate your abdomen to check for any abnormal sounds. These include:
The triangle of auscultation is a small region on your back where three back muscles meet. These muscles are the trapezius, latissimus dorsi and scapula. When you cross your arms and lean forward, these muscles thin out and the triangle of auscultation is better exposed. Your healthcare provider can hear your lung sounds more clearly when they place a stethoscope on this area.
Advertisement
The five auscultation points of the heart are areas your provider listens to with the stethoscope that helps them assess your heart health. They’re found at certain locations on your chest that are associated with heart valves. They are:
Although you may not be aware of it, your body makes noises all the time. You’re like a biological symphony of sounds. And sometimes, certain organs may be out of tune. These signs can tell your provider a lot about your health — or give them clues to help them diagnose potential conditions with more testing. If your provider discovers anything unusual, don’t be afraid to ask questions about their findings.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
